Those at Greater Risk of Overdose More Likely to Administer Naloxone.
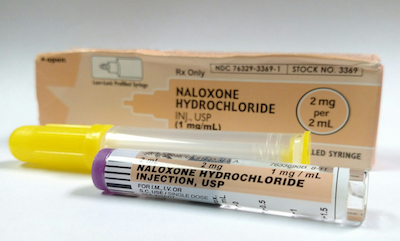 Naloxone, sold under the brand name Narcan, is a safe and effective antidote for reversing opioid overdose. The vast majority of bystanders who administer naloxone are themselves addicted to opioids, but little research has looked at the demographics of those who do intervene.
Naloxone, sold under the brand name Narcan, is a safe and effective antidote for reversing opioid overdose. The vast majority of bystanders who administer naloxone are themselves addicted to opioids, but little research has looked at the demographics of those who do intervene.
Now, a study co-authored by a School of Public Health researcher finds white and Hispanic people who use heroin and have overdosed or seen others overdose are more likely to administer naloxone than their black counterparts or those using prescription opioids.
The study, published in the Journal of Substance Abuse Treatment, used interviews with 468 people on admission to inpatient opioid detoxification at Stanley Street Treatment and Resources in Fall River, Massachusetts, in late 2015. The researchers found those at greater opioid-related mortality risk through heroin use, injected drug use, or history of overdose were more likely to have administered naloxone in the past year. However, none of the participants who used prescription pills and none of the black participants reported having administered naloxone.
“Unlike heroin users, pill users may be making only rare visits to settings where naloxone is freely distributed, such as healthcare facilities or needle exchange programs,” says study senior author Michael Stein, professor and chair of health law, policy & management. “Or perhaps they believe they’re at low risk of overdose.”
Nearly a quarter of participants who had ever overdosed had administered naloxone, compared to 9.8 percent of those who had never overdosed and 34.5 percent of participants who had previously seen an overdose reported administering naloxone in the past year. Participants who reported recent injected drug use were 19.5 percent more likely to administer naloxone than those who had not.
The vast majority of participants (82 percent) identified as non-Hispanic white, with the next largest group identifying as Hispanic. Although 18 of the study’s 20 non-Hispanic black participants used heroin, none of them had administered naloxone in the past year, compared with 14.5 percent of non-Hispanic white participants, 11.9 percent of Hispanic participants, and one-third of the 21 participants who identified as another race. Age, sex, and other demographics were not associated with significant differences in naloxone administration.
“We were surprised to find these stark racial differences in the use of naloxone,” Stein says. “It will be important to understand the causes in this region, and also to see if our result is repeated in other locations.”
The authors wrote the study findings may help physicians, policy makers, and public health officials better target their investment in distributing naloxone, and to determine whether perceiving a higher risk of overdose is an incentive to carry and use naloxone.
Co-authors of the study were Shannon R. Kenney of the Warren Alpert Medical School of Brown University and of Butler Hospital in Providence, Rhode Island; Bradley J. Anderson of Butler Hospital; and Genie L. Bailey of the Alpert Medical School and Stanley Street Treatment and Resources, Inc.