On Suicide.
 A study published recently in the Proceedings of the National Academy of Sciences received substantial attention. Anne Case and Angus Deaton showed that the death rate among white, non-Hispanic middle-aged Americans has recently risen, overturning decades of progress as part of a phenomenon that is unique to this racial group and that is distinct from trends in all other high-income countries. The authors noted that if the death rate among those aged 45 to 54 had continued to decline the way it had between 1979 and 1998, we would have avoided half a million deaths between 1999 and 2013. To put that in perspective, that is comparable to the number of lives lost to AIDS in the US.
A study published recently in the Proceedings of the National Academy of Sciences received substantial attention. Anne Case and Angus Deaton showed that the death rate among white, non-Hispanic middle-aged Americans has recently risen, overturning decades of progress as part of a phenomenon that is unique to this racial group and that is distinct from trends in all other high-income countries. The authors noted that if the death rate among those aged 45 to 54 had continued to decline the way it had between 1979 and 1998, we would have avoided half a million deaths between 1999 and 2013. To put that in perspective, that is comparable to the number of lives lost to AIDS in the US.
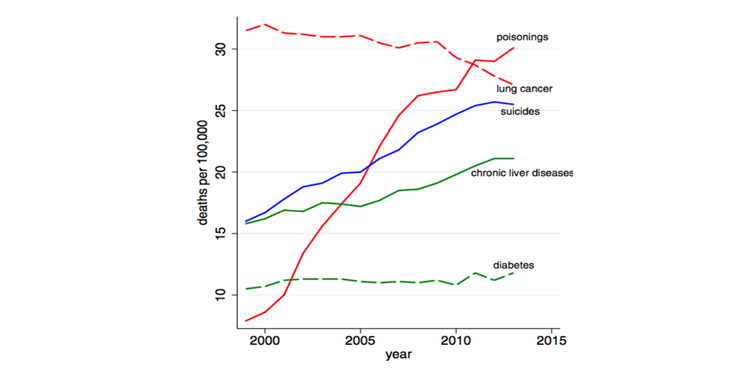
The paper suggests that there are two major contributors to this mortality increase: increases in drug use and suicide. Suicides among this group are represented by the blue line in the graphic below, second in rate of increase only to poisonings, the topic of a future dean’s note. The rate is highest among low-educated whites.
Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proceedings of the National Academy of Sciences 2015; 112(49): 15078-15083.
Although there has been, appropriately, quite a bit of media attention given to the problem of drug-related deaths recently—as we have seen drug overdoses, particularly from non-medical use of prescription opioids soar—there has been substantially less focus on suicides. I thought I would use the occasion of the Case/Deaton paper to comment briefly on suicides as a challenge to the health of populations.
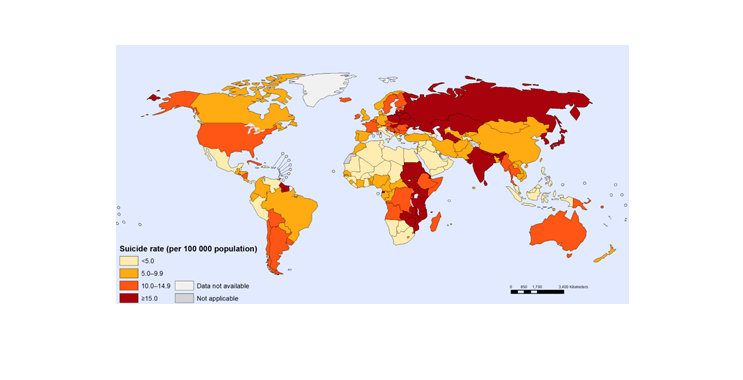
More than 800,000 people die each year from suicide, and it is estimated that about 10 times that number attempt suicide. In 2012, it was the second leading cause of death among people aged 15 to 29. Three-quarters of these deaths occurred in low- and middle-income countries (see Figure 2).
Mental Health: Suicide data. World Health Organization. Accessed January 15, 2016. http://www.who.int/mental_health/prevention/suicide/suicideprevent/en/
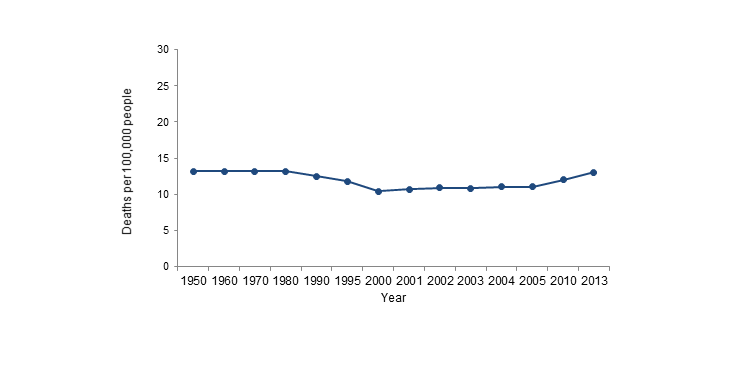
The challenge represented by suicides centers around two central aspects of the problem: its intractability and its unpredictability. Starting with the former, suicide mortality has been extraordinarily constant over many decades. Focusing on the United States, Figure 3 shows suicide deaths between 1950 and 2013, showing the overall stability of suicide death rates. This immobility unfortunately persists despite millions of dollars in expenditures in research and intervention efforts through a variety of both federal and non-federal sources.
Created from the Centers for Disease Control and Prevention, National Center for Health Statistics data. http://www.cdc.gov/nchs/
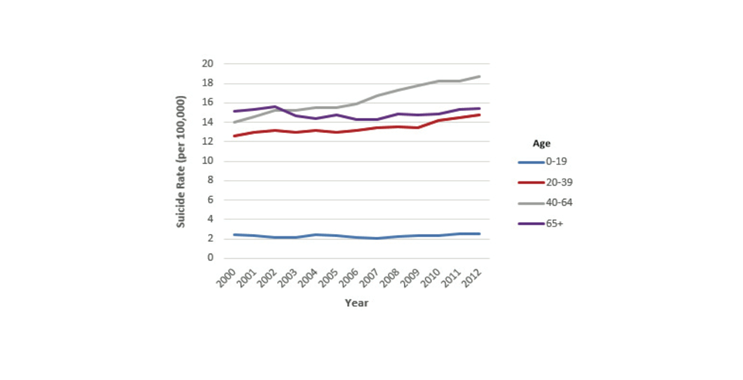
As noted earlier, suicides have come to attention recently out of a concern for rising suicide rates among less educated middle-aged adults. However, that paints only part of the picture. In the US, there are more than 41,000 deaths annually from suicide for a 13 per 100,000 rate. Figure 4 provides a picture of the demographics of suicide in the US, showing that indeed the highest rates have been among the 40-to-64-year-olds over the past 10 years, that youth suicide has been relatively stable, but that the rates among the 20- to-39-year-old age group have increased in recent years as well. Additionally, the majority of suicides occur among whites, with a rate of 14.75 per 100,000.
Suicide in the USA: Fact Sheet Based on 2012 Data (2014). American Association of Suicidology.
Attention has been drawn to particular subgroups of persons who are victims of suicide. Recent studies have demonstrated, for example, a clustering of suicides among students at Palo Alto area high schools, in one of the wealthiest areas of the country. Much more consistent attention has focused on the rising rates of suicide in military populations. In the past, suicide rates in the Army were lower than demographically matched civilian rates, but this changed by 2008, when the Army saw about 20 suicide deaths per 100,000 people compared to about 19 among civilians. In 2012, the number of deaths from suicide in the Army surpassed those from combat. Military personnel can face exposure to potentially traumatic events during deployment that can lead to disorders such as posttraumatic stress disorder, substance use disorder, and depression, and are often reluctant to seek help due to pressure and fear of losing their position. However, many soldiers also enter the military having already experienced suicidal thoughts, risk factors, and mental disorders in their lifetimes prior to enlistment. Separation from the military may also be associated with increased suicide risk, especially after a short amount of time and in absence of an honorable discharge.
The second feature of suicides that challenges our grasp on the problem has been the challenge to predict who may be a victim of suicide, with the vast majority of predictive models showing quite poor predictive validity at the individual level. What do we know about those in the general population who commit or attempt suicide? Importantly, a dose–response relationship has been suggested among a number of psychiatric disorders and long-term suicide risk. Perhaps most actionable, the majority of people who attempt suicide seek some kind of medical care in the months preceding their attempt, and about 80 percent of people contemplating suicide give some kind of sign of their intentions, including talking to loved ones about it. Additionally, 20 percent to 40 percent of people who actually complete suicide have attempted it in the past. Other proposed population-level risk factors for suicide include history of sexual abuse, financial strain or unemployment, and LGBT status and low family support, although these factors are important predictors at the population rather than individual level. Further challenging the field is the large number of studies that use suicidal ideation, reasonably enough, as a proxy for suicide for the purposes of work that aims to understand the drivers of suicide. Unfortunately, suicide ideation does not necessarily inform completion, and studies have suggested that the link between suicidal ideation and subsequent completion is weak.
The field of suicide prevention is growing, and there have been some potentially successful interventions aimed at decreasing suicide among certain groups documented. For example, one randomized control trial of suicide attempters in low- and middle-income countries compared individual sessions of education on alternatives to suicide, repetition, and referrals to usual care and saw significantly fewer deaths from suicide in follow-up among the treatment group. However, less has been done among groups that have not already attempted suicide.
Suicides remain, in sum, a substantial challenge to the health of populations, and one to which we have paid relatively little attention. One hopes that with a growing focus on population mental and behavioral health, commensurately greater interest in suicide can lead to insights and preventive approaches that dent what has been an intractable challenge for decades.
I hope everyone has a terrific week. Until next week.
Warm regards,
Sandro
Sandro Galea, MD, DrPH
Dean and Professor, Boston University School of Public Health
Twitter: @sandrogalea
Acknowledgement: I am grateful for the contributions of Laura Sampson to this Dean’s Note.
Previous Dean’s Notes are archived at: https://www.bu.edu/sph/category/news/deans-notes/