On Implementation.
 Before moving on to today’s subject, an acknowledgment that this marks the first Dean’s Note since entering a new and uncertain political era. Donald Trump’s inauguration as President of the United States is a milestone in our country’s history, and will likely have profound implications for public health. Respecting the strong feelings that this event has evoked, both positive and negative, I will take the next two notes to comment on how we might use this moment to further the goals of public health through a focus on promoting justice. Before tackling this theme, however, a note, perhaps fittingly, on implementation, and the complex work of mobilizing our aspirations in a changing, sometimes chaotic world.
Before moving on to today’s subject, an acknowledgment that this marks the first Dean’s Note since entering a new and uncertain political era. Donald Trump’s inauguration as President of the United States is a milestone in our country’s history, and will likely have profound implications for public health. Respecting the strong feelings that this event has evoked, both positive and negative, I will take the next two notes to comment on how we might use this moment to further the goals of public health through a focus on promoting justice. Before tackling this theme, however, a note, perhaps fittingly, on implementation, and the complex work of mobilizing our aspirations in a changing, sometimes chaotic world.
Since 2000, a number of studies have estimated the average time between research and implementation of action based on this research to be a period of about 17 years. On top of this nearly two-decade delay, the process of implementation is further complicated by the observation that many innovations never reach the point of continuous, widespread use at all. For example, in the area of infectious disease, the sometimes inconsistent performance of the directly observed treatment, short course (DOTS) strategy in fighting tuberculosis in Africa represents a case where an approach proves resistant to widespread implementation. I recently wrote about innovation and how we should actively embrace public health innovations, both technologies and novel approaches to policy, which can push our field forward. At the same time, I am painfully aware that innovation without implementation is folly, hallucination. Therefore, as a sequel of sorts to that piece, I would like here to highlight the key elements of successful implementation, taking into account the challenges of this process and suggesting some ways forward toward a more effective mobilization of our research and ideas.
We can perhaps ground our thinking in the formal work of implementation science, a growing field. Implementation science has been defined as the “scientific study of methods to promote the systematic uptake of clinical research findings and other evidence-based practices into routine practice,” in order to better link discovery with delivery of evidence-based interventions.
Applying this to health, we inevitably start with the delivery of medical care services, where much of the literature is grounded. Bollinger and Kruk recently conducted a review of innovations aimed at expanding access and improving quality of maternal and child health care services in low- and middle-income countries. They found that there was little overall guidance in the literature as to which interventions truly produced results, due in part to the lack of coherent methodological frameworks needed to direct the evaluation of interventions that seem promising but need further testing. This problem is not, however, unique to medical care, and it is not new. Going back 30 years, a 1985 article published in Harvard Business Review describes some of the challenges of implementing new technology in general, including resistance to change and the difficulty of promotion.
Jacobs and colleagues evaluated an innovation implementation framework that was originally developed for manufacturing, but has recently been applied to health care in the context of the National Cancer Institute’s Community Clinical Oncology Program (Figure 1). Their quantitative analyses confirmed the relationships highlighted in the framework, including the importance of the organizational climate for successful implementation of innovation in medical care.
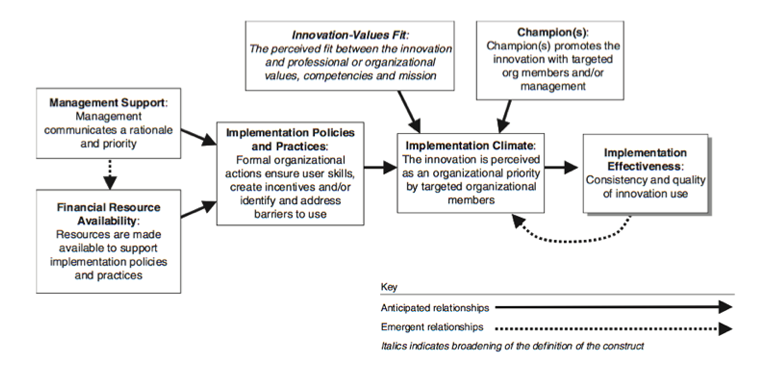
Helfrich CD, Weiner BJ, McKinney MM, Minasian L. Determinants of implementation effectiveness. Medical Care Research and Review. 2007; 64(3): 279—303.
Other frameworks for interventions have also been proposed, such as the earlier, slightly more linear one from Grol and Jones (Figure 2). The implementation science field has since evolved; recently, researchers have called for more complex approaches to implementation. This was particularly necessary in the Millennium Development Goals era, when it became clear that although more funding was available to try to meet these goals by reducing maternal and child mortality, as well as HIV, throughout the world, many new programs were not properly evaluated, making it difficult to know which interventions actually worked. In this context, Victoria and colleagues called for more analytic techniques, multi-level indicators, and transparency for large-scale programs.
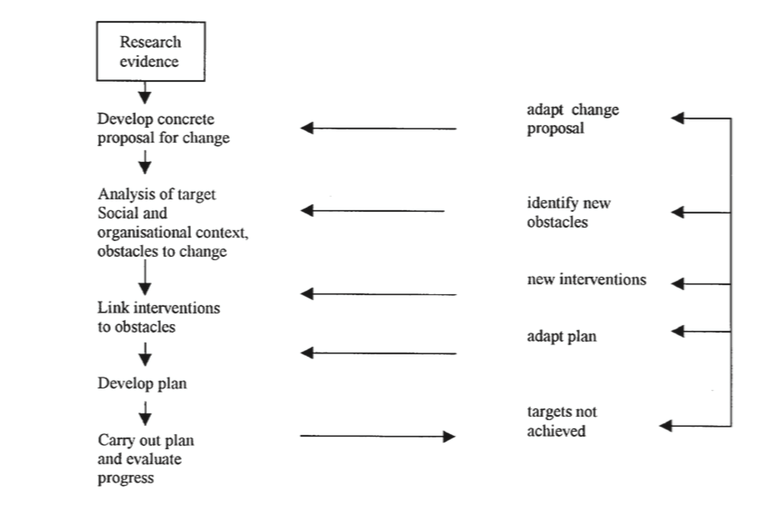
Grol R, Jones R. Twenty years of implementation research. Family Practice. 2000; 17: S32—S35.
What do I take from these frameworks? It seems to me that there are four principal components to successful implementation: political support, adequate funding, clear communication, and the effective management of logistics. There is also the matter of context, which is considered crucial to many of the frameworks that are applied to implementation science.
We can look to some of public health’s past successes to see how these assets contribute to achievement. For example, polio vaccination in the US and elsewhere has been successful due to careful attention to logistics, the financial backing of governments, and adaptive, well-planned communication. Implementation efforts have also been successful in the area of motor-vehicle safety, for much the same reasons. In 1999, the CDC listed improvements in motor-vehicle safety among the top public health achievements of the 20th century, touting a 90 percent decrease in annual US road deaths since 1925. This decline is due to a range of public health reforms, including legislation that set regulatory standards for roads and vehicles, and the introduction of seat belt laws. The implementation of these measures was bolstered by clear communication initiatives like road safety education campaigns designed to spread awareness of traffic rules. These efforts were also deeply informed by public health methodologies and research, pioneered by figures like William Haddon, the first director of the National Highway Traffic Safety Administration, who applied an epidemiological approach to the task of creating less hazardous roads. With government support, Haddon was able to mobilize his concepts of injury prevention, demonstrating the importance of political commitment to public health implementation.
I think these dimensions indeed represent what matters to implementation success. At core, though, there remains the role of context, without which I am not sure that any innovation can ever be implemented. The fight against polio and the push for safer roads are public health success stories not just because they represent a successful confluence of logistics, communication, funding, and political will leading to effective implementation. They are successes because they have managed to influence culture, nudging it in the direction of healthier populations. Childhood vaccination, regular seatbelt use—these have become expected behaviors in our daily lives, touching on something more fundamental than the rollout of a single program or even a national campaign. Rather, they help to create a society that is hardwired for greater well-being and more receptive to the work of public health.
Globally, we have seen how engaging with culture and social norms—foundational determinants of health—aids implementation. In Zimbabwe, for example, there has been a 34 percent decline in new HIV infections between 2005 and 2013, due, in large part, to cultural change around the issue of HIV, as well as the implementation of measures like condom distribution and the prevention of mother-to-child transmission with Option B+. In Cameroon, progress has been made against malaria through the distribution of more than 8 million long-lasting insecticide-treated bed nets; this progress has been driven by a media campaign that has helped to foster a “net use culture.”
For our interventions to be most effective, we must therefore understand, and adapt to, context, while at the same time maintaining fidelity to the core elements I have enumerated. It is a combination of a receptive context, shaped as it must be by a shift in values and expectations, that surrounds political support, adequate funding, clear communication, and the effective management of logistics that ultimately results in ideas becoming reality, in innovation being implemented, and in aspirations becoming better population health. Clearly our work then lies in improving all of these through our efforts to generate ideas and prepare the next generation to work with these ideas, and by acting to produce political will that allows the translation of ideas to action. At Boston University, we are also fortunate to have access to the Evans Center for Implementation and Improvement Sciences, which, under the co-direction of Mari-Lynn Drainoni, is available for consultation on how to best implement approaches to social science issues. Finally, we will, in April, be joined by JoAnn Kirchner, a leader in implementation science, who will help to inform our thinking on this subject as part of our Dean’s Seminar Series.
I hope everyone has a terrific week. Until next week.
Warm regards,
Sandro
Sandro Galea, MD, DrPH
Dean and Robert A Knox Professor, Boston University School of Public Health
Twitter: @sandrogalea
Acknowledgement: I am grateful to Eric DelGizzo, Laura Sampson, and Professor Mari-Lynn Drainoni for their contributions to this Dean’s Note.
Previous Dean’s Notes are archived at: https://www.bu.edu/sph/tag/deans-note/