Team led by Professors Ji-Xin Cheng and Chen Yang succeeds in suppressing seizure-causing neurons
By Patrick L. Kennedy
A Boston University team has discovered a new way of using microwaves to safely treat epilepsy and other neurological disorders. While it is still years away from clinical use, the technology was shown to reduce seizure activity in both in vivo and in vitro models of epilepsy, the team has reported in Science Advances. Developed under the direction of Moustakas Chair Professor of Photonics and Optoelectronics Ji-Xin Cheng (ECE, BME, MSE), and Professor Chen Yang (ECE, MSE, Chemistry), the device is a tiny microwave antenna implanted in the brain in a minimally invasive procedure.

“We are not cooking the brain,” says Cheng. The antenna, in the form of a split-ring resonator, receives a microwave from a hand-held transmitter and inhibits the problematic neurons—those that are firing excessively—that cause a seizure. “We use a very low dose so as not to injure healthy tissues,” says Cheng.
With this method, the microwave is concentrated at the target site, selectively suppressing the individual nerve that is acting up. While the study focused on epilepsy, the researchers believe the technology can also be applied to Parkinson’s disease and even chronic pain.

“We want to block action potential so that seizure or pain can be temporarily stopped in a drug-free manner,” says Cheng. Meanwhile, with a volume of less than 1.8 millimeters, the receiver can be inserted in a procedure much less invasive than current methods of epilepsy treatment, which involve deep brain stimulation.
“Microwaves haven’t been explored much for neuromodulation,” says doctoral student Carolyn Marar, the study’s first author. “Honestly, probably because it sounds scary. But our device is low power. It has no effect except at the site where it’s implemented,” where the effect is beneficial. “It’s a good middle ground because it has deep penetration and high spatial precision.”
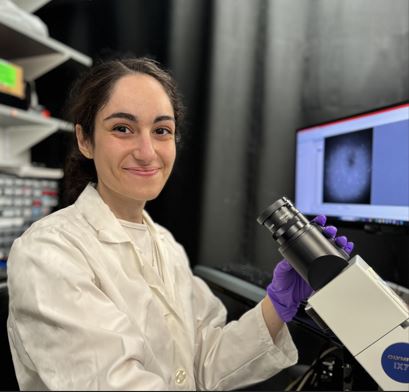
“I originally became interested in neuromodulation because my grandfather had Parkinson’s—he died of it,” says Marar. “That’s been a driving force for me getting into this field.”
The team included students in biomedical engineering, mechanical engineering, electrical and computer engineering, chemistry, and neuroscience. “This study is an excellent example of convergence of diverse expertise,” says Yang, co-lead of the team.
The team also received help from Ezra Cohen from the BU Chobanian and Avedisian School of Medicine for clinical guidance, and an expert at Children’s Hospital for development of the epilepsy model.
That convergent approach has been helpful, says Marar. “The project includes a lot of theoretical physics with the resonator, but also a lot of biology, working with neurons. As a biomedical engineer, it’s good to work with people specializing in those areas.”
