BU BME Graduates win 1st place in BMES-Medtronic Design Competition
Their device would treat one of the most common diagnoses in the neonatal intensive care unit.

BU BME graduates Meghan Griffin and Leen Arnaout, won first place in the 2021 BMES-Medtronic Design Competition for mechanical/electrical medical devices. Their project, A Wearable Solution for Treating Apnea of Prematurity, under the guidance of Professor Bela Suki, involved the design of a novel device that would effectively treat AOP, an understudied condition, and improve apneic infants’ clinical outcomes. The project also won first place in BME’s department-wide Outstanding Senior Design Project Awards for 2021.
Apnea of prematurity (AOP) is one of the most common diagnoses in the neonatal intensive care unit (NICU), affecting more than 85% of infants born before 30 weeks. Complications of premature birth — including AOP — are the leading cause of death for children under the age of 5. AOP-driven irregular breathing and systemic hypoxia can cause developmental delays and brain injury. A range of treatments are used to address AOP, including tactile stimulation, oxygen supplementation, NCPAP, and caffeine administration. These treatments require human intervention, are somewhat invasive, and may be associated with health risks and developmental delays. Devices using stochastic vibration to treat apnea exist but are not commercially available, and studies were inconclusive about their effectiveness.
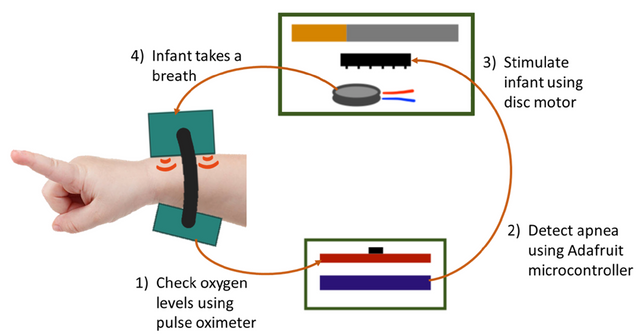
Preliminary research suggests deterministic stimulation is more effective in treating AOP than stochastic stimulation. Based on this knowledge, the team developed a safe, minimally invasive, and effective treatment for AOP in the form of a wearable device (bracelet). This device detects AOP-associated drops in SpO2 and responds with deterministic mechanical stimulation from a vibrating motor.
In addition to defining new stimulation schemes, the bracelet only stimulates the infant when apnea is detected, rather than continuously stimulating the child. The device was designed with two stimulation patterns, light and vigorous, and tested in rat apnea models, which confirmed the new stimulations significantly decreased the duration of apnea compared to unstimulated controls; apneic episode durations were reduced by 10-16%. Therefore, using this device to deliver the proposed deterministic stimulation would effectively treat AOP, and improve apneic infants’ clinical outcomes.
Both graduates have joined world-class BME-BIOE programs, at Minnesota (Meghan) and UC Berkeley-UCSF (Leen).