The Co-Infection of Hepatitis C and HIV.
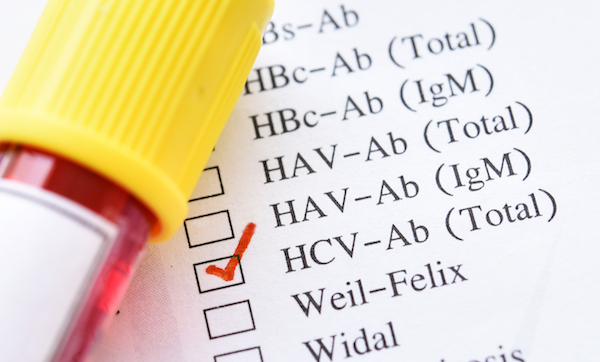
The Co-Infection of Hepatitis C and HIV
The HepCAUSAL Collaboration, co-led by a School of Public Health researcher, is the largest collaborative study of HIV and Hepatitis C co-infection, and aims to reduce the risk of Hep C reinfection and mortality.
The development of direct-acting antiviral agents (DAA) almost 10 years ago transformed treatment for hepatitis C virus (HCV) infection, effectively clearing the virus in 95 percent of people who received the medication.
Despite this major advancement, the blood-borne infection remains a major public health problem. Chronic HCV infection is common among people living with HIV, particularly among men who have sex with men (MSM) and people who inject drugs. Co-infection places patients at higher risks of morbidity and mortality from hepatic diseases (liver and cancer diseases such as cirrhosis and hepatocellular carcinoma), and extra-hepatic conditions (cardiovascular disease, kidney disease, and diabetes).
A new, international consortium formed by a School of Public Health researcher is leading the way on observational research of people who are co-infected with hepatitis C and HIV. The HepCAUSAL Collaboration is composed of investigators studying 11 cohorts of 25,000 patients in the United States, Europe, Canada, and Brazil. It is the largest collaborative study of HIV and hepatitis C co-infection, combining observational data and statistical methods to improve clinical decisions related to post-cure treatment of HCV, and to reduce the risk of re-infections and mortality among co-infected patients.
“Direct antiviral agents really revolutionized the treatment for hepatitis C infection when they became available in 2011 as a very effective treatment with few side effects,” says Sara Lodi, assistant professor of biostatistics and co-principal investigator of HepCAUSAL with Miguel Hernan, Kolokotrones Professor of Biostatistics and Epidemiology at Harvard T.H. Chan School of Public Health. “But there are still a lot of questions about what happens after people get cured—such as what problems do the still experience? Should we monitor them for liver-related issues, or the comorbidities that are typically associated with hepatitis C? Patients with HIV and hepatitis co-infection experience these morbidities more commonly and more severely.”
The idea for the HepCAUSAL Collaboration was borne from the HIV-CAUSAL Collaboration, a similar multinational initiative that has pioneered statistical methods to compare the effectiveness and safety of clinical strategies of HIV cohorts.
Among the first HepCAUSAL studies is one that Lodi led to estimate the proportion of co-infected individuals who are cured of HCV— determined by sustained virological response (SVR12), or the absence of the HCV in patients after 12 weeks of DAA treatment.
“This information can be difficult to acquire in real-world settings because it requires repeated testing, and patients often become less engaged over time in clinical trials,” Lodi says.
Using data from 4,223 individuals in six cohorts in the US and Europe, the researchers used inverse probability weighting to estimate the proportion of co-infected patients who achieved SVR12 after DAA treatment, while adjusting for baseline and treatment characteristics. They found that the estimates of SVR12 following DAA treatment were similar to those reported in clinical trials, “which indicates very high treatment success rates,” says Lodi.
The researchers are also applying causal inference methods to examine the independent effects of DAA treatment on study participants—rather than more traditional statistical methods that can only determine the relationship between two variables and can introduce biased estimates.
One of these studies, also led by Lodi, aims to better understand the long-term risks of HCV reinfection and liver diseases under the current DAA treatment guidelines for HIV and HCV co-infected patients. Understanding these risks will help inform the development of effective post-cure treatment, but there is limited research on the risk of reinfection, other comorbidities, and all-cause mortality among current HCV patients who receive DAA and the wide range of other health issues they may experience, such as frequent drug injection, poor kidney function, and insulin resistance.
Using causal inference, Lodi and the research team are estimating the cumulative incidence of HCV reinfection after successful DAA therapy, as well as quantifying the cumulative incidence of mortality, hepatocellular carcinoma, and liver transplants among participants after DAA therapy. They are also measuring the incidence of cardiovascular disease, kidney disease, and diabetes among the individuals after the recommended DAA treatment.
Most HIV and HCV co-infected individuals will likely receive DAA in the US and globally, so this information will guide post-cure management and enable patients to maximize the benefits of long-term DAA treatment, Lodi says.
“We want to be able to understand what the needs are for post-cure monitoring,” says Lodi. “If we find out that DAA drastically reduces the risk of hepatocellular carcinoma, then it means that patients won’t have to be monitored as closely as they used to be before they received DAA treatment for this type of cancer—and the same goes for cardiovascular disease and other comorbidities that typically affect these patients with hepatitis C.”