Lynne Stevens Memorial Program
About Us
Lynne Stevens was the Director of the Responding to Violence Against Women Program, and an Assistant Professor at the Boston University School of Medicine, Department of Family Medicine. Lynne was a clinical social worker who was a tireless advocate as well as clinician and researcher in the field of improving health care’s response to women experiencing violence. She specialized in evaluation of the quality of care offered in medical settings to women impacted by partner and sexual violence and died in 2009 at the age of 63. Working with such groups as the International Planned Parenthood Federation/Western Hemisphere and the United Nations Population Fund (UNFPA), she developed and implemented programs in many countries, including Nepal, Venezuela, Sri Lanka, Vietnam and Armenia. Educational materials that she developed for program developers and staff have been widely distributed by UNFPA, the CDC, and state anti-violence programs, and been translated into a variety of languages.
On moving to Boston University in 2005, she championed the integration into medical settings of programs responsive to victims of violence. She led initiatives evaluating and strengthening services for victims of violence in a variety of settings, including the Family Medicine Department’s Ambulatory Care Clinic and other Department practices, Manet Community Health Center, and Boston University’s student health services, and dental clinics. Lynne maintained active and substantial community commitments, supporting programs offering free yoga for women with issues of poverty, homeless, domestic violence or substance abuse histories. She also served as a member of the boards of directors of several domestic violence organizations in New York State and in Boston where she became Vice-President of the Board of Casa Myrna Vasquez.
To keep Lynne’s voice and work alive for us, the Family Medicine Dept started a dedicated annual Grand Rounds, inviting a speaker to remind, instruct and inspire us to improve the care we provide to the women who were her life work.. Thanks to a generous donation in Lynne’s memory, our ambitions expanded to include providing the kind of lovely lunch that she always offered her friends and inviting some of the wider community of service providers and coalitions that Lynne participated in across the campus and city.
An additional exciting development was the establishment of a grant program for a research or practice improvement project. Funded in 2011 for to provide annual $5000 grants for 5 years or the life of the fund, the focus is on evaluating, studying and improving care for women who experience partner and sexual violence receiving care in any of the hospitals, student health services and community health centers affiliated with Boston Medical Center or Boston University. This is a University-wide program, so that all faculty, staff, trainees and students of the University and affiliated services are eligible to apply if they receive endorsement by clinicians regarding clinical relevance. Like Lynne, we want to make sure that what we do makes a difference.
Paula Gardiner & Rob Saper went to the International Congress on Integrative Medicine Health Conference!
Click here to see all of the presentations by Paula Gardiner, Rob Saper, Chelsea Lemaster, Anna Lestoquoy, & Eric Roseen.
METHODOLOGY BOX LINK
METHODOLOGY BOX LINK
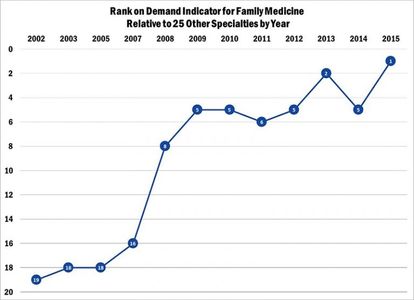
Methodology: Since the late 1990s, the Center for Health Workforce Studies, which is located at the University at Albany, State University of New York, has surveyed residents and fellows in New York State each spring as they complete their training. The survey asks several questions related to post-training plans and experiences finding a job. From these questions, CHWS developed a demand index. Using this demand index, they rank the relative demand for the 25 largest specialties: the specialty with the highest relative demand is ranked first and the specialty with the lowest relative demand is ranked 25th. CHWS has achieved consistency in the metric by using the same basic questions and methodology for the surveys throughout its 17 years of existence. With the excellent collaboration of teaching hospitals, a total of 2,897 of the estimated 5,308 physicians finishing a residency or fellowship training program completed the 2015 Exit Survey (55 percent response rate). To measure demand, each specialty is ranked on each of the following demand indicators:
- Percentage of respondents having difficulty finding a satisfactory practice position;
- Percentage of respondents having to change plans due to limited practice opportunities;
- Mean number of job offers received by respondents;
- Respondents’ perceptions of the regional job market (within 50 miles of their training program);
- Respondents’ perceptions of the national job market; and,
- Trends in median starting income.
Only residents and fellows completing training in New York State who had actively searched for a job are included in the survey, and they may or may not be representative of physicians training in the U.S. While New York State trains about 15 percent of all residents and fellows in the US, the job market they face may be very different than that in other parts of the country. We do know that New York State Graduate Medical Education has an unusually high percent of International Medical Graduates on temporary visas (about 18 percent), but they have been excluded from the demand index.
Table 1
“Boston docs call for more research, oversight on medicinal marijuana”
Some local doctors are calling for more scientific evidence to back marijuana’s medicinal value, and say close oversight is needed for pot dispensaries and prescribers to ensure that it does not get into the wrong hands.
“I think there’s a good place and time for use of marijuana,” said Dr. Katherine Gergen Barnett, a doctor at Boston Medical Center who specializes in integrative medicine. “But we haven’t as a society and as a medical institution done enough to oversee how people are getting prescribed marijuana.”
Click here to read the full article.
Congratulations to the grant writing team of Drs. Heather Miselis Brian Jack, Molly Cohen-Osher, Katherine Gergen-Barnett and Carol Mostow, LICSW for recently being awarded a 5 year HRSA Primary Care Training and Enhancement grant!
Congratulations to the grant writing team of Drs. Heather Miselis (Principal Investigator), Brian Jack, Molly Cohen-Osher, Katherine Gergen-Barnett and Carol Mostow, LICSW for recently being awarded a 5 year HRSA Primary Care Training and Enhancement grant for their project: Interprofessional Education and Expansion of the Primary Care Workforce: Developing a Collaborative Learning Model in Urban Underserved Patient Centered Medical Homes. This grant will fund a collaborative project between five training programs at Boston University: 1) Boston University School of Medicine Department of Family Medicine, including the FM residency program; 2) Boston University School of Medicine Physician Assistant Program; 3) Boston University School of Medicine; 4) Boston University School of Social Work; and 5) Boston University School of the Health and Rehabilitation Services, Sargent College, Department of Nutrition. The project will create an interprofessional learning collaborative that consists of BU CHAMPs (Boston University Community Health Alliance of Medical Professionals) and aims to inspire and train the primary care leaders of tomorrow to work in interprofessional teams in the setting of patient-centered medical home models of care in the community of Boston with each team drawing on the knowledge, talents, experiences, and perspectives of all members of BU CHAMPs.
Facilitators and Barriers to the Integration of Mind–Body Medicine into Primary Care
 Chelsea McGuire, MD,1 Jonathan Gabison, BA,2 and Benjamin Kligler, MD2,3
Chelsea McGuire, MD,1 Jonathan Gabison, BA,2 and Benjamin Kligler, MD2,3
Abstract
Purpose: To improve understanding of the facilitators and barriers affecting the integration of mind–body medicine (MBM) into primary care and describe the experiences of mind–body primary care providers.
Methods: The authors conducted a qualitative analysis of semi-structured telephone interviews with mind–body primary care providers selected via a maximum variation sampling strategy.
Results: Four main themes emerged: (1) MBM is an approach to patient care as well as a set of modalities, (2) time and reimbursement pose significant challenges to MBM, (3) support for MBM in one’s practice setting is a key facilitator, and (4) commitment to MBM comes from personal experience. ‘‘Insufficient time’’ was the most highly ranked barrier among survey respondents. Interviewees described innovative strategies to overcome barriers, including customized intake forms, MBM training for staff, MBM group visits, and discounted referrals for low-income patients.
Conclusions: While increased MBM and self-care training for providers may facilitate the integration of MBM into primary care, systematic changes are needed to decrease time pressures on providers and incentivize patient wellness. Despite barriers, providers are using innovative strategies to provide mind–body primary care in diverse practice settings.
Click here to read the full article that is published in the "Journal Of Alternative And Complementary Medicine".
Center for Teaching & Learning Expands Efforts
BU Center for Teaching & Learning fellows: (back row, from left) Jonathan Hibbard, Christophor Cavalieri, Cheryl McSweeney, Kaija Schilde, Pary Fassihi, Peter Zink, and Scott Marr; (front row, from left) Sophie Hochhäusl, Gouri Gupte, center director Matthew Trevett-Smith, Bruce Anderson, and Rosina Georgiadis; (not pictured) Anthony Mecham. Photo by Jackie Ricciardi
Matthew Trevett-Smith sent an email in April inviting faculty to apply for a six-week summer fellowship at the Center for Teaching & Learning designed to inspire creative changes in classrooms across BU. And while the fellowships include a $6,000 stipend, new center director Trevett-Smith didn’t expect a big response given that it was already late in the semester and both he and the center were unknown quantities. “I thought 5 or 10 responses would be a good number,” he says.
Instead, 40 proposals came in from faculty members in nine schools across both campuses. The applicants’ objectives ranged from improving class videos to fine-tuning collaborations among students. Trevett-Smith chose 12, he says, because a dozen is the most you can have in a comfortable and cohesive faculty learning community, “particularly if you want to get everyone around a single table.”
And that was exactly what he wanted. Weekly group conversations over lunch and dinner at Silber Way were high points of the six-week program, which ran concurrently with the first summer term.
Click here to read the full story.
“Integrative Health Group Visits As Core Delivery Strategies”
by John Weeks, Publisher/Editor of The Integrator Blog News and Reports
Integrative health group visits was the topic of an April 28, 2016 grand-rounds webinar with the Academic Consortium for Integrative Medicine and Health, the organization of 68 academic medical centers promoting the integrative model. The two speakers were Katherine Gergen-Barnett, MD (pictured right) with Boston Medical Center (BMC), and Ilana Seidel, MD (pictured below) from George Washington University Medical School.
The growing exploration of “integrative health group visits” as core delivery strategies has developed from a need to consider strategies for cost savings as well as a number of other reasons including the following:
- A focus on education and empowerment in integrative health and medicine.
- Evidence that adults learn best when they are not merely being passive recipients
- The whole person philosophy that success in creating health is ultimately in the hands of the individual seeking care rather than the practitioner who provides it
Gergen-Barnett opened the recent webinar by speaking to the power of the approach: “The idea of group visits is that we as human beings are built for community – and when we get sick we are often alone […] Group visit theory is that patients working together as a group can manage conditions better [and] not about the provider being in the room.”
Click here to read the full article.
“Effective Feedback in the Education of Health Professionals”
Rebecca F. Lara, MD Kris M. Mogensen, MS, RD, LDN, CNSC Jeffrey F. Markuns, MD, EdM
Abstract
Clinical educators of health professions training programs are often underprepared for their teaching roles due to a lack of formal training in educational methodology. The emphasis on competency-based education in the health professions has led to a re-evaluation of the standards for a competent clinical teacher. Feedback is an important aspect of nearly all learning theories. The effectiveness of feedback
relates to its double-barreled approach that focuses on both the cognitive and motivational aspects of learning. Feedback should be related to progression toward competency to promote self-motivated
learning. Both the tone and perceived intention of feedback affect how a learner incorporates and uses
such information. Descriptive feedback on the performance of tasks is the most beneficial. Characteristics of effective feedback include the creation of a receptive environment, focus on behaviors, specificity, comparison to a standard of competency, timeliness, ensuring an appropriate
amount so as to not overwhelm the learner, and encouragement of self-directed learning. Faculty
development interventions targeted toward learning to provide appropriate feedback are critical in improving the educational process.
Click here to read the full article.
2016 APHA PCC Gabby/Gabe Abstract Acceptances
- Abstract #366453
Title: "Assessing the Relationship between Social Support & Preconception Care (PCC) Risk Prevalence in young African-American Women”
Authors: Rock, N, Jack, B, Bickmore, T, Damus, K, Yinusa-Nyahkoon, L, Gardiner, P, Penti, B, Semenya, M, St. Fleur, M, Alhelo, H, Julce, C, Adigun, F, & Jackson, C.
Oral Presentation
- Abstract #365782
Title: "Health Information Technology: Guidelines for Web-based Educational Programs Targeting Young, African American Women
Authors: Yinusa-Nyahkoon L, Adigun F, Gardiner P, Damus K, Julce C, St. Fleur M, Semenya AM, Penti B, Woodhams E, Bickmore T, Jack B
Roundtable Presentation
- Abstract #365922
Title: "Mitigating Mental Health Preconception Risks for Black Women with the ‘Gabby System'"
Authors: St. Fleur M, Semenya AM, Yinusa-Nyahkoon L, Jack B, Damus K, Julce C, Martin, M.
- Abstract #362730
Title: "Is Perceived Discrimination Associated with Preconception Health Risk Factors in Black Women?"
Authors: Semenya AM, Jack B, Bickmore T, Yinusa-Nyahkoon L, Julce C, Penti B, St. Fleur M, Damus K.