With the motto “Advancing Science to Heal the World,” the BU stem cell scientists who founded the Center for Regenerative Medicine (CReM) could be pegged as starry-eyed idealists. Or, they could be seen as scientific pioneers who are willing to sacrifice some glory and profit for the advancement of science.
What CReM codirectors Darrell Kotton, Gustavo Mostoslavsky, and George Murphy are, undisputedly, is venturesome researchers who are willing to buck the long-standing practice of jealously guarding scientific breakthroughs. The trio’s “open source biology” describes their desire to share their discoveries with almost anyone, with the conviction that more brainpower will speed medical progress. In August, their efforts won a five-year $2.7 million grant from the National Heart, Lung, and Blood Institute’s Division of Lung Diseases, to make CReM’s bank of lung disease–specific induced pluripotent stem (iPS) cells available to researchers across the country.
Open source science is unusual in any field, but in a field as competitive as regenerative medicine, it is downright radical. One young researcher training at CReM recently approached Kotton, a School of Medicine professor of medicine, seeking advice on how to answer an outside request for a vial of stem cells that took several years and hundreds of thousands of dollars in federal grants to develop. The obvious answer, the trainee assumed, was to tell the researcher to wait until the report on the discovery was published.
Kotton saw it differently. “Our mission is to decrease the burden of human suffering on the planet, help patients, and advance new knowledge,” he told the trainee. “If this competitor of ours has the same goal, then we’re obligated to share this cell vial with them, because that’s going to achieve our mission…which is not to get credit and to stroke our egos.”
“Here’s the thing that nobody talks about,” says Kotton. “If you behave in this way, people in our community quickly get the idea that the BU/Boston Medical Center CReM are the good guys of science. At some point, the equation gets so lopsided that people almost feel embarrassed that they’re not sharing with you and so they tell you stuff, and the whole field starts to move forward.”
That was the theory anyway, and now, in fact, CReM founders are being asked by increasing numbers of researchers to collaborate on grants; foundations have begun to recognize that funding a CReM project very probably means that resulting knowledge, expertise, and reagents will be shared with other academic or nonprofit laboratories without restriction or exclusivity.
“I can’t emphasize enough how unique that was for the community,” says Mostoslavsky, a MED assistant professor of gastroenterology. “We have dozens of emails that testify to that, saying, ‘I must tell you this is the first time in my 30 years of being a scientist that someone replied and sent me stuff the same week I asked for it.’”
Still, Mostoslavsky says, there is a fine balance between freely sharing their work and protecting it once research has advanced to the clinical stage. “It’s very expensive—no academic institution can support it—so we do need a company to move forward,” he says, which also means they’ll need patented protection of intellectual property.

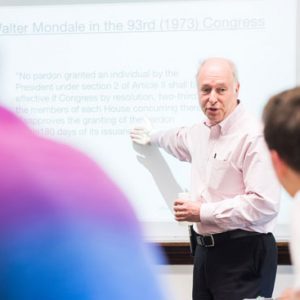
Stem cell scientists Gustavo Mostoslavsky (from left), Darrell Kotton, and George Murphy are willing to buck the long-standing practice of jealously guarding scientific breakthroughs. Photo by Jackie Ricciardi
SCIENTIFIC SOUL MATES
Kotton, Mostoslavsky, and Murphy met as Harvard postdoctoral fellows in the lab of stem cell scientist Richard Mulligan, who is famous for his rigorous research and forthright style of mentorship. “It was more of a sink-or-swim methodology, where you really had to prove yourself,” says Murphy, a MED assistant professor of medicine. “Coming out of there, we were battle-tested and bombproof.”
Kotton, Mostoslavsky, and Murphy have followed the rapid advance of stem cell biology since 2006, when scientists at the University of Kyoto reprogrammed adult cells to develop into what are called induced pluripotent stem (iPS) cells—which resemble embryonic stem cells and can be used to create heart, lung, liver, or other cells. A tinkerer at heart, Mostoslavsky was fascinated by the Kyoto process, but felt he could go one better. In 2008, he developed a more efficient tool to generate stem cells, called the stem cell cassette (STEMCCA). BU patented the tool, and it has become the industry standard.
In 2010, with STEMCCA and multiple publications under their belts, the trio established a virtual Center for Regenerative Medicine, with its own website, seminar series, and iPS cell bank carrying branded labels.
As the number of stem cell biologists, physician-researchers, and biomedical engineers grew on both BU campuses, the affectionately labeled CReM brothers felt it was time to pitch a physical center to BU President Robert A. Brown, who firmly backed the idea. Boston University and Boston Medical Center (BMC) invested jointly in the endeavor, and in November 2013, CReM opened in its newly remodeled space at 670 Albany Street.
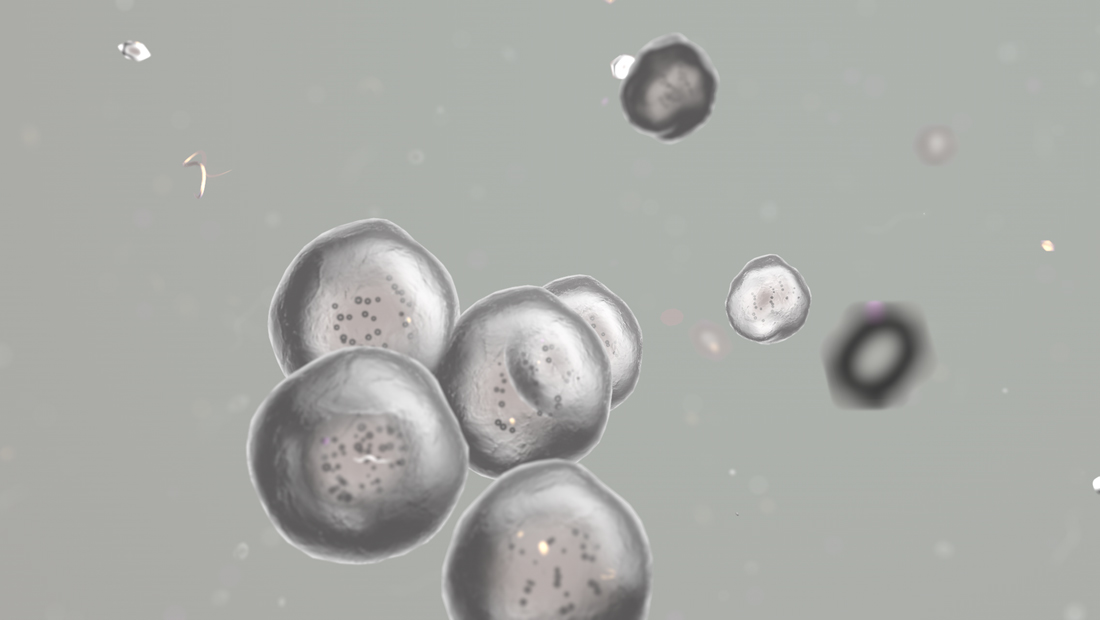
In the video above, CReM founders discuss how they use induced pluripotent stem (iPS) cells in their labs.
CReM’s mission is to advance stem cell research and regenerative medicine for the treatment of patients, in particular those at BMC, with diseases such as cystic fibrosis, emphysema, sickle cell anemia, and amyloidosis. Investigators collect blood or skin cell samples, usually from patients at the Alpha-1 Center, the Center of Excellence in Sickle Cell Disease, and the Amyloid Center, and reprogram them into iPS cells.
“Any cell can be reprogrammed,” says Mostoslavsky. “It’s a true biological rejuvenation. The cells really go back in time.” Researchers now have the ability to coax iPS cells—which uniformly carry a patient’s genetic mutations—into their desired cell line, such as lung, liver, or blood. (CReM’s iPS cell bank stores at least 13 such cell lineages.) Mostoslavsky says the resulting cells are “still a work in progress,” compared to those found in nature, but the process allows researchers to watch how an iPS-derived lung cell develops the early stages of cystic fibrosis. What took years to unfold in a patient takes days in the lab.
CReM investigators can screen drugs against patient cell lines to determine which medications are most effective for a specific genetic mutation—the “clinical trial in a test tube,” as Murphy calls it. “In theory,” he says, “you could develop therapies that are molded specifically for a particular patient with a particular disease.”
Developmental biology and drug screenings are now CReM’s bread and butter, but its founders keep in mind what they call their long-term “Apollo projects,” such as genetically engineering iPS cells to correct patients’ mutations. The resulting healthy cells could be cultured and multiplied to regenerate a transplantable organ that wouldn’t be rejected by the patient’s body.
Kotton has been collaborating with a team of Massachusetts General Hospital researchers using a technology called lung decellularization and recellularization, which strips the organ of its cells and repopulates it with genetically engineered copies that lack the patient’s original mutation. Theoretically, the reprogrammed cells could multiply, fill the lung’s scaffolding, and someday be used for transplantation. Kotton, who thinks it will be possible eventually to re-create lungs via 3-D printing technology, is collaborating on this with Christopher Chen, a College of Engineering professor of biomedical engineering.
Meanwhile, Murphy dreams of brewing blood. “The human body makes 2.5 million red blood cells every second of every day,” he says. “How does one contend with that from a research platform?” He thinks they will be able to “harness molecular cues” that exponentially increase the amount of artificial blood they can produce in vitro. Such a discovery could eliminate the need for blood donation in the United States and—even more urgent—in developing countries, where the practice is not widely accepted.
Another one of Murphy’s Apollo projects is boutique blood, or the development of small batches that could be produced for people who suffer from sickle cell anemia or the blood disorder beta thalassemia and require transfusions of rare blood types.







































Related Stories
CReM Honored for Sharing Stem Cell Lines
Team wins award from Association of American Medical Colleges
CReM Stem Cell Researcher Is Innovator of the Year
MED’s Gustavo Mostoslavsky invented tool facilitating cell production
BU Wins Life Sciences Capital Grants
Support for regenerative lung medicine, training for biotechnology careers, biophotonics start-ups
Post Your Comment