On August 2, the first of two sickened American health care workers was flown from Africa to a special containment unit at Emory University. Despite the risk of infection, medical personnel continue to travel to West Africa to help bring under control the worst Ebola outbreak on record, which according to the World Health Organization (WHO) has killed more than 900 as of August 6. WHO plans to spend $100 million to fight the outbreak, and the Centers for Disease Control and Prevention will send 50 more disease control workers. In this weeklong Special Report, BU Today talks to Boston University researchers in several fields about why medical personnel confront the risks; the ethical and political dilemmas presented by the outbreak; how the virus kills; efforts to design effective therapies; and other aspects of this unprecedented outbreak of Ebola.
Elke Mühlberger, associate professor of microbiology at the School of Medicine, is one of a small group of microbiologists around the world who are trained to work with Ebola and similarly deadly viruses in Biosafety Level 4 (BSL-4) labs. She began her work 20 years ago at the BSL-4 lab at Philipps University of Marburg, in Marburg, Germany. Mühlberger, whose research is funded by the National Institutes of Health, the Defense Threat Reduction Agency, and Boston University, is director of the Biomolecule Production Core at BU’s National Emerging Infectious Diseases Laboratories (NEIDL).
BU Today spoke with Mühlberger about why Ebola kills so quickly and what it’s like to work with this virus—why she feels no fear—and about her hopes that her lab’s research will help in the development of antiviral drugs and vaccines against Ebola virus and other known and unknown emerging infectious diseases.
BU Today: You’ve been working on Ebola and similar viruses for 20 years. What is special about Ebola? Why does it kill people so quickly?
Mühlberger: This is not completely understood. What we do know is that Ebola virus messes with our immune system. We are not able to fight off the viral infection in our body quickly enough to avoid becoming dangerously ill. Once infected, our body is flooded with Ebola virus particles. We do not really understand why we are not able to fight off Ebola virus infection.
It is believed that humans are not at all adapted to Ebola virus. It lurks in remote areas in central Africa in the rain forest, and possibly in West Africa, too, as we have learned from the current outbreak. Usually humans are not exposed to it.

Click to enlarge. The life cycle of Ebola virus. Bats are believed to be both reservoirs and hosts for Ebola. Of the five identified subtypes of the ebolavirus genus, four are capable of human-to-human transmission. Initial infection in humans results from contact with an infected bat or other wild animal. Image courtesy of the Centers for Disease Control and Prevention
How do humans get exposed to Ebola in the first place? Where does the virus live initially?
We know that in the case of Ebola’s close relative, Marburg virus—an equally dangerous virus which causes the same disease as Ebola virus—its natural host is a fruit bat, Rousettus aegyptiacus. It is believed that the natural hosts for Ebola virus are also fruit bats. So if humans come in close contact with infected animals—for example by handling bush meat—the virus can be transmitted, or jump, into the human population.
What do we know about how this Ebola outbreak in West Africa began?
The first case in the current Ebola virus outbreak was identified as a 2-year-old child in the village of Meliandou in Guéckédou prefecture, Guinea, who got infected and died in December 2013.
There is some speculation that this child might have been exposed to fruit bats. The occurrence of this species of Ebola virus, Zaire Ebola virus, in West Africa was completely unexpected. Previously, this virus was believed to be endemic to central Africa.
Before this horrible outbreak, there was only a single case of Ebola virus infection reported in West Africa, in the 1990s. The patient was an ethnologist who performed behavioral studies of chimpanzees in the Taï National Park in Ivory Coast. Some of the chimpanzees got infected with Ebola virus and died, and the researcher contracted the virus when she handled the dead animals. However, the Ebola virus species in the Ivory Coast incident is considerably different from the one causing the current outbreak.
How does this connect to your research?
One of our research goals is to understand how a protective immune response against filoviruses—Ebola and Marburg viruses are classified as filoviruses—works. In collaboration with the research teams of Gustavo Palacios at the US Army Medical Research Institute of Infectious Diseases (USAMRIID), Jonathan Towner of the Centers for Disease Control and Prevention (CDC), and Thomas Kepler here at BU, we perform comparative studies of the immune responses to Marburg virus infection in bats and humans. Our part of the project includes in vitro work—using bat and human cells.
In contrast to humans, fruit bats infected with Marburg virus do not become ill. With the hope that we will identify novel targets for human therapeutics, one of our projects is to identify the exact mechanisms that allow bats to fight Marburg virus infection.
You are trained to work with these viruses in BioSafety Level 4 (BSL-4) labs, which have the most highly regulated safety standards and precautions in place. You worked with these viruses for years at the BSL-4 lab at Philipps University of Marburg, in Germany, including while you were pregnant…
Yes, I worked through both my pregnancies. I felt absolutely safe in the BSL-4 lab. Fortunately, we had pretty big BSL-4 suits in Marburg and I still fit in with my huge belly. My boys are now 13 and 9 years old and both are very proud of having been in the BSL-4 suite before they were even born.
What we’re hearing about the Ebola outbreak is so scary. We understand that you’ve worked with Ebola and similar viruses in highly contained settings that bear no resemblance to the situation facing health care workers on the ground in West Africa. But what is it about the BSL-4 lab setting that makes you feel safe—you’re not even a little afraid?
I have a great deal of respect for Marburg and Ebola viruses. But I don’t fear working with these viruses.
I always keep in mind how deadly they are when handling them in a BSL-4 lab. However, BSL-4 labs are some of the safest places on earth and working with dangerous viruses in these labs is strictly regulated. We use appropriate personal protective equipment (PPE), including state-of-the-art BSL-4 laboratories, fully-enclosed positive pressure suits, and three pairs of gloves, to make sure that we do not get infected and that the environment is protected.
The BSL-4 lab at BU is not operational yet. There are four BSL-4 trained people in my lab, including myself. To get our necessary BSL-4 work done, these BSL-4 trained lab members commute to off-site BSL-4 labs in San Antonio, Texas, and Hamilton, Montana.
Viruses do not ask for permission to cross borders. We need to be prepared.
I have a great deal of respect for Marburg and Ebola viruses. But I don’t fear working with them.
There aren’t many microbiologists who are trained to work with these viruses and have been doing it as long as you have. How did you get into this?
Just by chance… When I was a student at the Philipps University of Marburg, Germany, I was looking for a slot to do my diploma thesis in biology. I met a young researcher who had just finished his MD/PhD and was on the way to establish his own lab to work on the weirdest virus ever—Marburg virus. The guy was Heinz Feldmann, who is now chief of the laboratory of virology at the National Institutes of Health/National Institute of Allergy and Infectious Diseases (NIH/NIAID) Rocky Mountain Laboratories in Hamilton, Montana, and one of the most respected experts in the field of filovirus research.
What interested you about this virus?
When I started to work with Marburg virus in Heinz’ lab, almost nothing was known about it. Everything we did was new and exciting, and after all these years in the field, everything we do still feels new and exciting.
My diploma project was to sequence one of the Marburg virus genes, the glycoprotein gene, which is responsible for attachment and entry of the virus into cells. I sequenced like crazy, and the encoded protein became longer and longer because I could not find an end to the gene. I was completely desperate until it became apparent that I was working on the wrong gene. It turned out that I wasn’t sequencing the glycoprotein gene but instead was sequencing the polymerase gene. This mistake was the foundation for my own research projects when I became an independent PI with a strong focus on the viral polymerase and the replication and transcription strategies of Marburg and Ebola viruses.
Can you tell us more about your work on the Ebola virus?
My lab works on two angles to study the Ebola virus. First, we are interested in understanding what the virus needs to replicate inside an infected cell. Like many other viruses, Ebola virus brings its own genome replication machinery into the cell. If we understand how this machinery works, we can identify targets for antiviral compounds that block viral replication. This approach has been used successfully for other viruses, such as herpes viruses and HIV.
Second, we are interested in the antiviral response to the Ebola virus infection at the cellular level. Ebola virus infects specific cells of the immune system that are needed to fight the virus at an early stage of infection. In these cells, Ebola virus blocks antiviral pathways and reprograms the cells in a way that they are not able to respond to the infection effectively.
On top of this, the infected cells are used as vessels to transport the virus to almost all organs of the body, where it infects additional cells. This leads to a so-called systemic infection with the devastating consequences for which Ebola virus infections are notorious.
Therefore, our goal is to identify antiviral pathways that can be activated in Ebola virus–infected cells, which would lead to the destruction of the infected cells before the virus can spread further. For example, we have tested an antiviral drug similar to one that was developed by Todd Rider at MIT several years ago and is currently being tested in animals. This drug selectively induces a suicide program in virus-infected cells. We showed that it kills Ebola virus–infected cells without harming uninfected cells. If the infected cells are eliminated, the virus cannot spread through the body anymore.
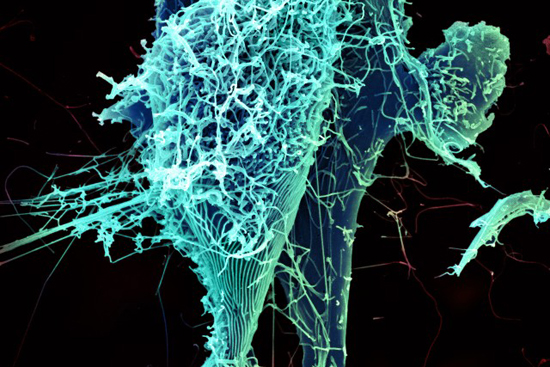
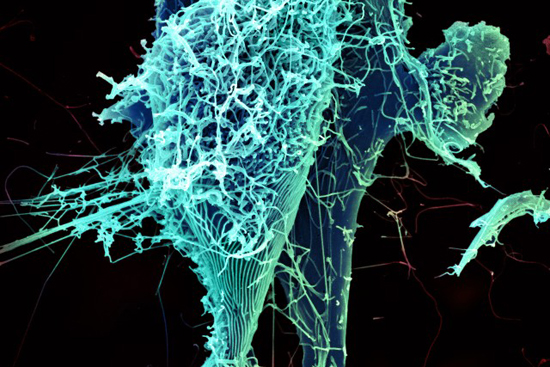
This electron micrograph shows string-like Ebola virus particles shedding from an infected cell. Photo courtesy of National Institute of Allergy and Infectious Diseases
Do you eventually hope to do experiments in animals?
I am a molecular biologist, and this work was done in cell culture. As soon as the NEIDL is operational, we would like to collaborate with researchers who work with animals to test approaches like this in animal models.
Does the Ebola outbreak in West Africa add to your sense of urgency about your own research?
This is a truly horrible outbreak and it makes me sad because many of the deaths could be avoided. Ebola virus is transmitted by body fluids. It is not airborne. That makes it relatively easy to stop transmission of the virus by following simple protective measures. With this in mind, it is very disturbing that so many health care workers became infected and died because of the lack of appropriate personal protective equipment (PPE). Having a therapeutic or vaccine in hand could help save so many lives, especially among the health care workers who devote their lives to treat patients.
Recently, there has been great progress in the development of antivirals and vaccines against Ebola virus, which have been tested in animal models. These include the ZMapp antibody cocktail made by Mapp Biopharmaceutical Inc., which has been used to treat Dr. Kent Brantly and Nancy Writebol. I deeply hope that the severity of this outbreak will help push the initial testing of these vaccines and therapeutics into human trials so that they could be used in future outbreaks.
If we could back up a bit, for those of us who are just learning about Ebola, here is a really basic question: What is a virus?
Viruses are particles of nucleic acids, either RNA or DNA, which are surrounded by proteins and sometimes additionally by lipid membranes. With few exemptions, viruses are very small, about 100 times smaller than bacteria. Most importantly, viruses have a parasitic life style and must infect living cells to reproduce. They hijack cellular machineries to amplify their genomes and produce their own proteins and membranes.
Is Ebola an RNA virus? And why is it considered a filovirus? What does that mean?
Yes, Ebola is an RNA virus. It belongs to the family of filoviruses. This name comes from the Latin word filum, which means thread. Ebola virus particles are rod-shaped and are surprisingly simply organized. The small viral RNA genome, which consists of only 19 thousand nucleotides—human genomes consist of billions of these nucleotides—is tightly associated with only seven proteins and encased in a membrane.
One of the viral proteins sticks out of the membrane and can bind to receptors on the surface of cells. Binding to these receptors helps the virus enter the cell. Inside the cells, Ebola virus replicates itself. Then the new viral particles leave the cells and are ready to infect fresh cells. At some point, the infected cells get exhausted because they have to provide all the material needed to form the virus—and they die. However, Ebola virus–infected cells survive for a pretty long time, making it easy for the virus to spread throughout the body of the infected host.
So you mean you can’t have Ebola virus for years and not know it…like with HIV?
Exactly. Ebola virus causes an acute infection. The infection lasts for about two weeks and then it is over. If the patient is lucky, he or she survives, but unfortunately, in most of the cases, the patients die. The case fatality rates of Ebola virus infections can be as high as 90 percent, depending on the virus species. So unlike other viruses, including HIV, Ebola virus does not persist in the infected patient. In this aspect it behaves more like the influenza virus. You get ill and a couple of days later it is over—one way or another.
Tomorrow: Why Researchers Need to Work with Deadly Pathogens. Read all stories in our series, “Battling Ebola” here.







































Related Stories
Battling Ebola: Tracking the Virus
Current Ebola outbreak defies earlier models
Battling Ebola: NEIDL’s Role
Researchers eager to unlock secrets of emerging pathogens
Ebola Research Begins at NEIDL
After years of review, lab receives first BSL-4 pathogen
Post Your Comment