On August 2, the first of two sickened American health care workers was flown from Africa to a special containment unit at Emory University. Despite the risk of infection, medical personnel continue to travel to West Africa to help bring under control the worst Ebola outbreak on record, which has killed more than 900 people to date. The World Health Organization plans to spend $100 million to fight the outbreak, and the Centers for Disease Control and Prevention will send 50 more aid workers. In this weeklong Special Report, Bostonia talks to Boston University researchers in several fields about why medical personnel confront the risks; the ethical and political dilemmas presented by the outbreak; how the virus kills; efforts to design effective therapies; and other aspects of this unprecedented outbreak of Ebola.
How have African governments and the West responded to the Ebola outbreak in Liberia, Guinea, and Sierra Leone that has likely infected more than 1,700 people and killed over 900, according to the World Health Organization (WHO)? About as well as possible, given huge impediments, says Davidson Hamer, BU ethicist and infectious disease physician. He says more resources are needed to develop vaccines and treatments for the killer virus—even if it means diverting money earmarked for combating other infectious diseases.
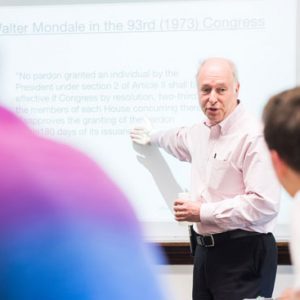
A professor of global health and medicine at the School of Public Health, Hamer has overseen 50-plus studies in developing nations and is currently based as a faculty member at BU’s Center for Global Health and Development. He codeveloped and has taught a course on debates, including ethical ones, about how best to control infectious diseases. It will be taught this fall by a colleague, SPH Associate Professor Jean van Seventer. Hamer is also the principal investigator with GeoSentinel, a global network of travel clinics and hospitals that monitors global trends in the incidence of disease among travelers and is funded by the Centers for Disease Control and Prevention (CDC) and operated by the International Society of Travel Medicine.
As the governments of the three African nations and the CDC and WHO struggle to contain the outbreak, “My biggest concern is a spread to other countries” in Africa, says Hamer. “Nigeria is one of the most densely and heavily populated countries on the subcontinent. If it spreads there, we could have a very large-scale epidemic.”
Bostonia spoke with Hamer about the Ebola outbreak during a brief visit to BU; he will be returning later this month to Zambia, where he currently lives.
Bostonia: Have the efforts to control the epidemic met your ethical criteria?
Hamer: The authorities have been having a hard time controlling this. Part of the problem is behavior-change communication: this area has never had Ebola before.
It’s spread across borders, which is unusual. There are misperceptions and fears about seeking treatment. That’s causing [infected people] to leave towns and infect relatives. My speculation is people fear that if they go to a health center, they’re going to get sick there. It’s not a complete misperception, but it makes it hard to contain the disease when people are running the other way.
You’d generally give good grades to the response and say that the CDC and WHO are doing the best they can under the circumstances?
I think that’s true. It’s very challenging.
Some have suggested the world would be doing more if the victims were citizens of a white, industrialized nation.
I guess I partly agree. There would be major attention and intensive efforts to control the outbreak through many means [in a developed country], including education. That said, CDC and WHO have been very proactive. The CDC put out a lot of announcements [about] no non-essential travel.
Can medical and aid workers be given enough protection to be on-site without undue risk? Is it appropriate for some to pull out?
The answer is yes to both. Ebola is spread through blood and body fluids, but some studies suggest aerosol transmissions can occur. Personally, I would want respiratory precautions as well as a full body suit that couldn’t be punctured. That’s expensive. They should be pulling people out who can’t have that protection.
What do you think about shipping some of the infected patients out of affected areas for treatment?
When somebody’s really sick with this, they need maximal intensive care support, which is generally not available [in the outbreak regions]. But the risk of moving someone—they may die in transit, or infect health personnel—there’s a risk there. Bringing treatment to the field makes good sense.
What about the remoteness of the outbreak areas?
It’s a good point. One option would be to set up a central facility in a capital, like Freetown [Sierra Leone] or Monrovia [Liberia]. There are also portable field stations that could be adapted and brought into remote areas. These are approaches that have been tried [elsewhere] that allow you to treat anybody who’s been infected.
Some villagers threatened to attack doctors, whom they consider purveyors of the disease. How possible is it to counter such fears?
It’s not easy, and it requires effective community education. Working with traditional and community leaders to make them a spokesperson is an effective way. You’re more likely to counter some of the animosity. Having worked extensively in Africa, we’ve done this in Zambia for some of our community health projects.
Does colonialism play a role in spreading distrust of Westerners?
Liberia has been independent for quite a while. It’s internal dictators that have done damage there and in Sierra Leone. Guinea is different. There’s definitely animosity toward the French because of the way they treated their colonies.
How well have the African governments performed in this crisis?
I think Liberia and Sierra Leone have very broken health care infrastructures. Both countries were torn by civil wars. The end result is whatever health systems they had were destroyed, and it’s taking a lot of work to build them back. The road infrastructure in both is not so great, either.
If we invest more in combatting Ebola, will that mean fewer resources to eradicate other infectious diseases that might affect more people?
Ebola virus has a potentially very high fatality rate, and it can spread rapidly, as it has now. Even though the threat of introduction to the United States is relatively minimal—and hospitals would limit the spread or curtail it altogether—the problem is that it tends to occur in places where you don’t have good infection control measures in place. And burial practices in some parts of Africa—they wash out various cavities of the body—lead to substantial risk of exposure to any pathogens a [deceased] person might have. If this were to hit a country that’s more densely populated, like Nigeria, it could spread rapidly.
The overall burden of Ebola compared to something like malaria is tiny in terms of number of infections, number of deaths. The better analogy is to rabies, which is almost 100 percent fatal. Despite the fact that Ebola’s a rare thing, it’s been cropping up. We need to spread attention to it, even though we may divert resources from other infectious diseases.
Tomorrow: Working with a deadly virus. Read all stories in our series “Battling Ebola” here.





































Related Stories
Battling Ebola: Tracking the Virus
Current Ebola outbreak defies earlier models
Battling Ebola: Heading Into the Outbreak
NEIDL’s Nahid Bhadelia to care for patients, share expertise
Going Public with Ebola
NEIDL director says scientists need to engage with the public about the disease
Post Your Comment