Jerry Savory has had a hard life. The 57-year-old with a salt-and-pepper beard and a broken nose has struggled with alcoholism and drug use since he was a teen. He’s suffered from seizures since he was in an accident at age 25. And he’s still recovering after a car hit him two years ago.
Medical issues like these would spell misery for anyone, but for people like Savory, who is homeless, a group whose mortality rate is at least four times that of the general population, the misery is compounded. Savory considers himself lucky, however, in one regard: he is treated regularly at the Boston Health Care for the Homeless Program (BHCHP), which is staffed in part by first- and second-year School of Medicine student volunteers.
“Every time I’ve been here, every time I leave, I be all right,” Savory says slowly, his brow furrowing as he sits in a BHCHP exam room.
Savory was one of several patients examined late one night by MED students enrolled in the Homeless Health Immersion Experience, a noncredit, service-learning program started last spring by two medical students interested in gaining early clinical experience and exposure to a vastly underserved population.
“BU medical students don’t really have much experience with the homeless population,” says Raagini Jawa (MED’14), who cofounded the elective program with Alec Peniche (MED’14). “This is a great way for students to understand a different subset of ailments and issues.” Peniche says students also appreciate the opportunity to build rapport across classes, and to pass along “little clinical pearls” of wisdom.

Jawa is a cofounder of MED’s Homeless Health Immersion Experience.
Jawa and Peniche developed the program with Suzanne Sarfaty, MED assistant dean of academic affairs and director of international health programs and an associate professor, and with BHCHP doctors Jennifer Brody and Mardge Cohen, who agreed to supervise the students.
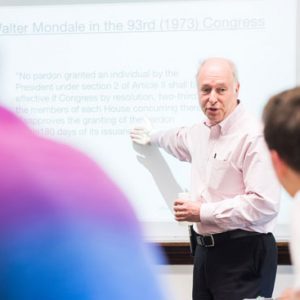
The pilot for the program was last spring, with 12 first-year students and 12 second-year students, who worked in pairs and rotated through an outpatient clinic and a respite center on a monthly basis. While the first group gained valuable patient interviewing skills, the second practiced physical examination techniques and acted as friendly mentors to their less-experienced peers. After each exam, the students presented a patient’s case to Brody or Cohen, who gave them pointers on technique and explained how homelessness influenced the patients’ medical conditions.
Since the full-fledged program launched in September, Jawa and Peniche have expanded it to include BHCHP-affiliated medical residents, who give mini-lectures to students about issues related to homelessness and health care. The cofounders also partnered with MED’s Outreach Van Project, which serves the homeless population once a week in East Boston.
The Boston Public Health Commission reports that in 2011, nearly 6,650 people were homeless in Boston, and just over half of them were single adults living on the street, in shelters, in transitional housing, or in treatment facilities.
Jim O’Connell, a MED assistant professor, who founded BHCHP in 1984, puts the number higher; he believes that 25,000 Bostonians are homeless for some period of time each year. His organization serves more than 11,000 people a year through street outreach or at its Albany Street headquarters, which has a pharmacy, a dental office, an outpatient clinic, and a 104-bed medical respite center.

First- and second-year MED students collaborate throughout each exam in BHCHP’s clinics.
Incredibly gratifying experience
Hours after closing time for most doctors, Cohen sits in a BHCHP exam room with three medical students who just saw their first patients. “The idea was for you to feel comfortable learning about someone who’s had a lot of vulnerabilities,” she says. “Knowing how to care for, and care about, the most vulnerable attests to the type of people you are. Many medical students do not want to take care of such people. You will see that it’s an incredibly gratifying experience.” Cohen then asks the students to present their patients’ cases.
Nahiris Bahamon (MED’15) and Stephanie Donatelli (MED’15) take turns describing the condition of a 46-year-old male. He’s a self-described alcoholic with neuropathy, acid reflux, arthritis, and a long history of personal tragedy. Both his parents were alcoholics. One brother, a drug user, died of AIDS. Another died of cirrhosis. His firstborn died of SIDS. He has a history of depression and anxiety, and although he’d been sober for two years, he wants to return to detox after a recent relapse.
“He’s very self-aware,” Donatelli says. “We didn’t even have to ask that many questions.”
Cohen laughs. “Your empathy shows, which is very important,” she says. “He elicits that in us.” She discusses the impact personal trauma has on health, the genetics of alcoholism, and the post-traumatic stress disorder the patient likely suffers from because of his child’s early death. “Do you think that could be someone you know?” she asks. “Or do you think it happened to him because it was going to happen?”
Bahamon reviews the patient’s complicated life history and suggests that “he was set up for failure.” Donatelli agrees, adding that each time he rallied, something beyond his control knocked him down.
Cohen emphasizes the importance of being there for a patient when he falls, as many times as he falls, and to look for small victories in his daily life—like the desire to get treatment for alcoholism. “Hopefully he’ll go into a program and stay,” she says.
Across the hall in another exam room, Savory is pleased to have a warm meal and a place to stay for the next few days. He’s uncannily calm about the ill turns his life has taken and draws from a deep well of faith—something he says his grandmother instilled in him as a kid attending church every Sunday.
“No matter how bad people treat you, just leave it in the hands of God,” he says. “The only thing you can do is just pray for ’em.”







































Related Stories
MED’s Bauchner Elected to National Academy of Medicine
Plum honor for Journal of the American Medical Association editor
School of Medicine Launches Military Health Center
Coordinating the University’s military-focused research and service projects
Patient Navigators Improve Delivery of Care for Breast Cancer Patients
BMC program reduces cancer disparities by addressing barriers to timely care
Post Your Comment