How Point-of-Care Testing Will Transform Healthcare
Catherine Klapperich’s first target: HPV
“A private little revolution any woman can easily buy at her drugstore.”
That’s how a 1978 ad described the new-to-market home pregnancy test. Today, that revolution is replayed in millions of American bathrooms every year—so many that it hardly feels revolutionary anymore.
But Boston University engineering professor Catherine Klapperich understands just how powerful it is to have direct access to your medical information. She’s working to make that “little revolution” a lot bigger through simple, portable tests for conditions like HPV, malaria, and chlamydia that patients can use worldwide.
“In a fragmented healthcare system like ours and like many around the world, you have to be your own advocate,” says Klapperich, who also serves as director of the Center for Future Technologies in Cancer Care (CFTCC) and associate dean for research and technology development at the College of Engineering. “Being the best advocate you can be requires information. Information is power.”
Klapperich’s tests are called point-of-care diagnostics. They are designed to be as easy and portable as those pee-on-a-stick tests, but the chemical machinery inside them far outstrips the strip. Her tests zero in on specific sequences of DNA, called nucleic acids, that single out the cause of infections. Nucleic acid tests usually require lab equipment that costs tens of thousands of dollars; Klapperich’s miniversions fit in your hand and give results in a matter of minutes.
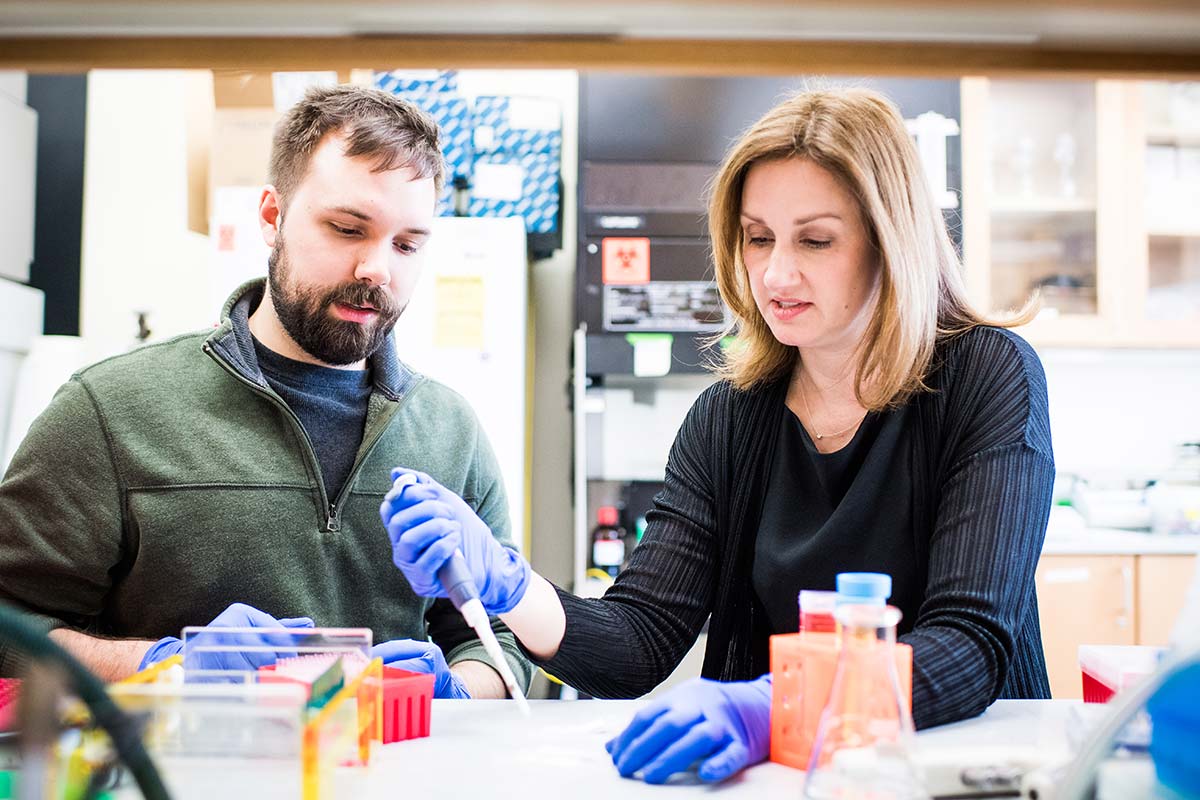
In Klapperich’s lab, students and researchers are developing tests for malaria, chlamydia, gonorrhea, and more. “There are all kinds of applications” for paper-based testing, says Klapperich, here with PhD candidate Justin Rosenbohm (ENG’20). “And it makes the students who come work for me a much broader group of people.” Photo by Jackie Ricciardi
One of Klapperich’s first targets is human papillomavirus (HPV), which is responsible for almost all cervical cancers. Cervical cancer is highly treatable when it’s caught early. That’s why, in places like the United States, where nucleic acid testing is readily accessible, doctors advise women to get regular HPV tests. (In fact, the new tests are beginning to replace the old standard, the pap smear.) A woman who tests positive for a cancer-causing HPV strain will be closely monitored so that if cancer starts to grow, she can get treated right away.
In parts of the world without these resources, doctors typically diagnose HPV based on a visual exam of the cervix. That means more false positives and more false negatives, says Klapperich, and thus more cervical cancer death and disease for women in low-resource countries, where some 85 percent of new cervical cancers and cervical cancer deaths occur. In India, for example, cervical cancers kill 74,000 women each year—a third of the world’s deaths from the disease. Almost every one of those cancers started out as HPV, a sexually transmitted infection (STI).
“STIs have such a huge impact on women’s health, and they don’t have to,” says Klapperich. “Some lead to sterility and other complications, and because many are asymptomatic, women are being harmed without knowing it. Knowing your status, being able to test yourself, puts the power back into the hands of the woman.”
As for why she has taken up this work, Klapperich says: “If women don’t pioneer in this area, then who will?”
Curiosity and collaboration
Designing and building the devices requires a blend of biology expertise, engineering know-how, and fundraising finesse—plus relationships with doctors and hospitals. Klapperich has a gift for bringing together people with all of these skills, and then bridging the gaps between them.
Many people look at Klapperich’s career—the titles, the awards, the patents—and imagine her as a little girl, taking apart the VCR, building robots in the basement, and analyzing pond scum with a mini-microscope. But that’s not who Klapperich was. She planned to major in journalism, but switched to engineering after seeing a lab demonstration of cement hardening under an electron microscope. (It was cooler than it sounds.) She wants students to know that the key to a great career isn’t fate or brilliance, but curiosity and persistence. She wants them to know they don’t have to ace AP chemistry to be an engineer. (She didn’t even take it.) And she wants them to know that doubt is allowed.
“It’s a real joy working with her,” says Jose Gomez-Marquez, cofounder of the Cambridge, Mass., device maker MakerHealth. “With other researchers, it’s often this gamesmanship of, ‘How can I show you I’m smarter than you?’” But that isn’t Klapperich, he says, and her intellectual unpretentiousness makes it easier to solve complex problems.
“As a collaborator, she truly tries to get everybody involved to their fullest potential,” says Mario Cabodi, an ENG research assistant professor of biomedical engineering, who has been working with Klapperich since 2010. “She’s all about giving people opportunities.”

Klapperich with student Marjon Zamani (ENG’20) in the lab. Klapperich wants students to know that in science, tenacity and curiosity are more important than acing AP chemistry. “At every step of the way, it’s all about persistence: staying in, not quitting,” she says. Photo by Jackie Ricciardi
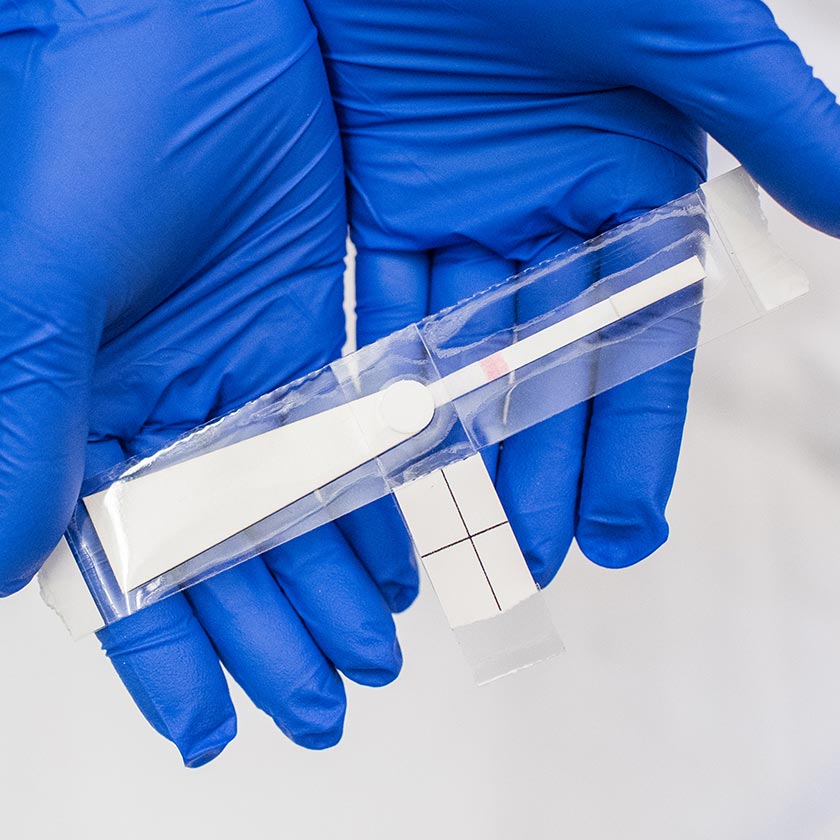
Klapperich’s point-of-care HPV diagnostic is a device about the size of a candy bar and can detect the virus at a patient’s bedside in about 30 minutes. Here’s how it works: A doctor—or even the patient—collects a sample of cells from the cervix, then mixes the sample in a test tube with a chemical that cracks open the cells and makes their freed DNA clump together. Then, a doctor or technician dabs the resulting liquid onto a strip of testing paper and uses alcohol to rinse away the proteins, carbohydrates, fats, and other cellular debris. What’s left behind is pure DNA. If a patient’s cells are infected with HPV, that DNA will include the distinctive sequence of the virus, and the result will show up on the test strip: one line for negative and two for positive, just like a pregnancy test.
MakerHealth started producing the tests in January 2018.
Downsizing (in a good way)
How does Klapperich cram a whole lab’s worth of diagnostic equipment onto a handheld test strip? “Because we’re trying to make things smaller, faster, and cheaper, we go back to the drawing board with all these old protocols and we try to reinterrogate them, to figure out what’s necessary and what’s not,” she says. “It goes back to Engineering 101: How can I make this work best with the least amount of cost, or the least amount of steps, or the least amount of moving parts?”
Klapperich’s team has already shown that the test works well in the lab, but once a test gets out into the real world, there’s more room for human error. The team is tweaking the packaging, so the tester only has to touch the paper strip twice: once to drop in the sample and again to start the reaction. That will reduce the odds of cross-contamination and false positives.

A sample is applied to Klapperich’s paper-based HPV test. If the sample contains DNA from potentially cancer-causing HPV, two lines will appear on the test strip. Photo by Joseph Lee Photography
The same basic technique—swab a sample onto paper, wash away the cellular scrap you don’t need, heat the strip up, and read out the result—can be used to create tests for a huge variety of diseases. Researchers in Klapperich’s lab have made sexually transmitted infections like HPV, chlamydia, and gonorrhea their first targets; third-year biomechanical engineering graduate student Nikunja Kolluri (ENG’20) is adapting the technique to test for malaria.
Because nucleic acid dissolves easily in water, Klapperich says, it is also possible to use just the first two steps of the procedure to sample and preserve DNA for testing at a lab elsewhere. Just add water to the dry, preserved sample and it is ready to be analyzed.
That’s useful for diagnostics that require more than a simple yes or no readout. People taking antiretroviral drugs for HIV, for example, have to get regular blood draws to measure how much HIV is in their blood—a number called viral load. “With HIV, you want to know not only is the virus there, you want to know how much virus is there, and is it more than the last time I tested this person?” says Klapperich.
Regular viral load testing is difficult for people living in remote communities. They often have to travel long distances to get to a clinic, then wait days or weeks for their results. To eliminate that travel burden, some healthcare workers take the tests to their patients. That means fanning out, collecting blood samples, refrigerating them, and transporting them back to a central lab.
In 2011, Klapperich and Gomez-Marquez went to Nicaragua, where they saw firsthand the challenges of viral-load testing. A sophisticated lab in Managua could handle the testing, she remembers, but they saw how easy it was for a sample to “spoil” on the way there. “It has to stay cold, it has to be preserved, it has to be handled correctly, and it has to get there within a certain amount of time,” she explains. Samples from the far east of the country weren’t weathering the trip. “Jose and I started brainstorming on that problem immediately.”
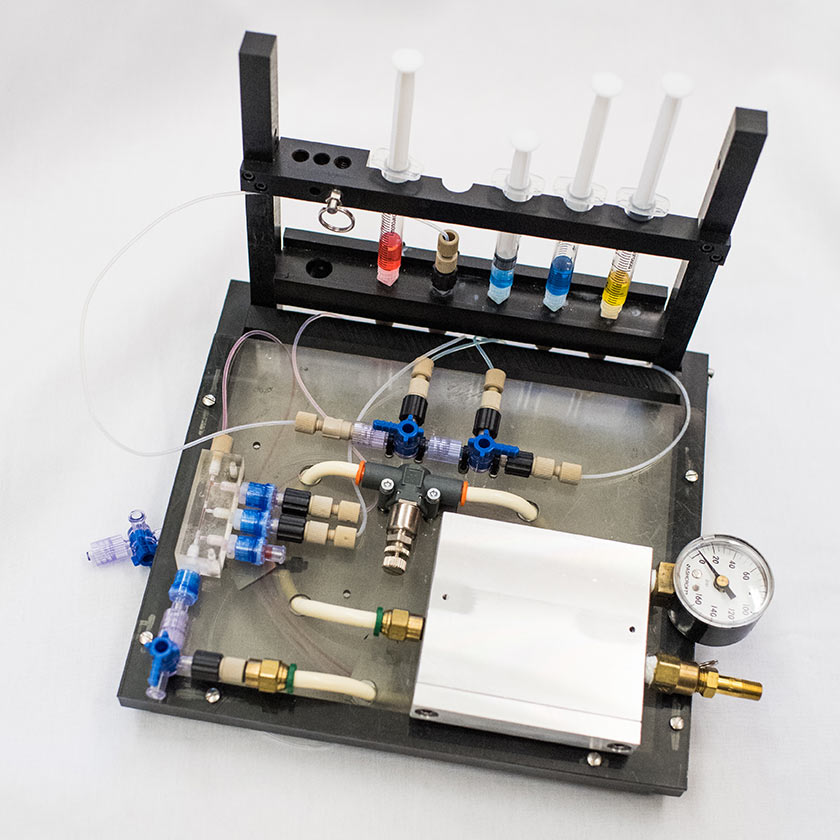
Now, they are working on a way to collect blood samples, store them on a small strip made of layers of paper and flexible plastic, and preserve them so that each one can be tucked into a plastic baggie with a packet of silica gel (like the one that comes with a box of new shoes) and shipped off to a lab, without the need for refrigeration along the way. “You make it smaller, you make it lighter, you take it out of the cold chain, and then it becomes something that you could theoretically mail,” says Klapperich. Her group has already shown that samples preserved in this way will last at least two weeks.
An early HPV test prototype from Klapperich’s lab (left) was the size of a small suitcase; the latest, paper-based version (right) would tuck neatly into a pocketbook. Photo by Jackie Ricciardi
Klapperich and Gomez-Marquez are working on a way to turn their prototype strip, which they’ve dubbed SNAPflex, into something that can be manufactured on a larger scale. Their design inspiration: tape.
“Tape is made everywhere in the world—Brazil, Chile, India,” says Gomez-Marquez, who also directs the Little Devices Lab at MIT. Because tape is made on standard reel-to-reel machines, tape-based test strips could be made in existing factories with little modification, he says. And the test strip housing wouldn’t just look like tape: it could actually be tape, specifically plumber’s tape. Like plastic kitchen wrap, plumber’s tape sticks to itself without any adhesive. All it takes to seal up the test is another layer of tape over the top.
“When I go to foreign countries, nurses know down to the last penny how much things cost,” says Gomez-Marquez. Plumber’s tape, he says, is cheap and accessible, and because it is familiar, it is less intimidating to use: “That’s why we call it DIY diagnostics. If I can do it, I can teach everyone else how to do it.” In November 2017, the collaborators won a $100,000 grant from the Gates Foundation to advance the new device.
The “DNA-to-go” technique has applications Klapperich had never even imagined before. “I get calls all the time from people who work in all kinds of fields,” she says. One call came from a researcher studying wild primates. The scientists wanted to study blood-borne infections in the animals, but couldn’t take blood vials, which are considered biohazards, out of the nature reserve. Klapperich’s technique seemed like the perfect solution: they could extract DNA from the animals’ blood, preserve it, and take it back to the lab for testing without any danger.
“The most exciting discussions that I have are with scientists who have really good ideas but don’t necessarily have the time or the bandwidth to work on them. There’s no ceiling on the number of things that people who are in these different labs, in these different countries, could do with it,” says Klapperich. “And to me, that’s much more exciting: enabling the work of other people.”
In the United States, there is no shortage of diagnostic labs, but point-of-care testing is still a booming multibillion-dollar business, and consumers are increasingly seeking the convenience and privacy of at-home testing. Think of it as the old-fashioned house call, minus the doctor.
“Walk into CVS, you can buy drug tests, you can buy pregnancy tests, you can buy cholesterol tests,” Klapperich says. And while checking your cholesterol from the comfort of your living room in Boston might be (literally) thousands of miles away from getting a bedside HPV test at a Chennai hospital, to Klapperich, they are variations on a theme. “It’s giving people their health information and breaking down whatever barrier is there to get them their health information.”
Comments & Discussion
Boston University moderates comments to facilitate an informed, substantive, civil conversation. Abusive, profane, self-promotional, misleading, incoherent or off-topic comments will be rejected. Moderators are staffed during regular business hours (EST) and can only accept comments written in English. Statistics or facts must include a citation or a link to the citation.