Area p53
Cancer research demystified.
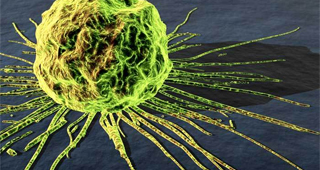
Weeds prevent grass, plants, and flowers from growing in your backyard. The longer one lets weeds grow and prosper on nutrient rich soil, the more parasitic they become. If weeds are permitted to prosper, they not only become difficult to remove, but it becomes more difficult to prevent subsequent weed growth. Cancer cells are like uncontrollable weeds and make it difficult for the body to carry out its normal processes.
Professor Richard C. Lewontin of Harvard University blames the existence of weeds on human activity, such as forest fires and construction projects, which creates ideal environments for weed growth. Cancer cells can similarly arise from human activity.1 These cells originate as normally functioning cells; however, upon exposure to excess radiation, chemicals (e.g. hairspray), inhaled of toxins (e.g. cigarette smoke), or acquisition of unstable genes from previous generations, these normal cells sustain damage to their DNA. These mutations cause a breakdown of the cellular mechanisms that control cell growth and division. Once these regulatory checkpoints have been irrevocably damaged or duped, the cell divides uncontrollably, thereby becoming cancerous. Although it is commonly believed that only a few mutations can generate cancerous cells, it is in fact a buildup of mutations and a subsequent breakdown of regulatory mechanisms that yield these aggressive and invasive cells.
What Needs to Get Fixed?

Cancer begins when a small group of cells acquire some mutation (by means of radiation, environmental factors, toxin, old age) that affects them in such a way that control of cell division is lost. It is not just one mutation that results in full-blown carcinoma. Only upon sustaining several mutations does a cell become cancerous cells.2 Cancer cells exhibit loss of stratification, contact inhibition, and cell cycle control. Stratification is a property of normal cells whereby cells precisely organize in three dimensions along the contour of whatever tissue they construct. For example, cookies placed over the surface of a table to have an even, 1-layer surface would be normal stratification. Contact inhibition is another natural property of normal cells which allows cells to grow and divide in a two-dimensional fashion until they come in contact with another cell. Cells that acquire mutations lose this ability and eventually go on to develop less structural organization, and begin growing on top of one another.3 Cells are normally guided through mitosis via a checkpoint process that involves proteins known as cyclins. When cyclin regulation breaks down, mutations accumulate. A loss of cyclin-dependent regulation permits the perpetuation of mutations to the progeny of the mutated parent cell. As these mutations accumulate, normal cell growth becomes impaired. Eventually, cells begin to lose control over their division, which leads to a mass of wildly growing cells with virtually uninhibited growth and proliferation.4
Cancer Biochemistry: Solving Big Problems with Small Steps

Biochemical pathways that are targets for drugs fall under two general classes: tumor suppressing and oncogenic. Tumor suppressor pathways do exactly that: in a normal schema, when cells are damaged (i.e. DNA damage) these proteins and pathways become activated in such a way that prevents the mutations from being perpetuated in future progeny of the cell. These avenues include programmed cell death (known as apoptosis) or growth arrest (senescence).5 Examples of tumor suppressor pathways include p53 (tumor protein 53) and Rb (retinoblastoma protein). Oncogenes, which have a precursor form known as proto-oncogenes, become activated when the cell requires growth and division. Unfortunately, when cells acquire a significant amount of mutations, they can turn the precursors into active oncogenes and thereby have a permanent “on” switch, which forces constant cell division. Examples of oncogenes include Ras, myc, and several tyrosine linked kinase receptors (such as epidermal growth factor receptor, and platelet derived growth factor receptor). Many therapies that target oncogenes attempt to shut down the active oncogenes by deactivating the oncogene or by inducing cell death5.

Much of the biochemically driven research in the last few decades has focused on reactivating the downstream targets of tumor suppressor proteins, such as p53. For example, the Xiao lab at Boston University School of Medicine is focused on several proteins that share functional similarities to the p53 protein, namely p63 and p73. As mentioned, p53 is critical for maintaining stability of the genome in normal cells.6 Proteins such as p63 and p73 have been classically defined to play a role in epithelial stratification (p63), and neurological development (p73). However, structural similarity of the p53 gene in both the transactivation domain (a domain in which, when transcribed, yields a higher rate of gene expression) and DNA binding domain to the p63 and p73 isoforms suggest that these two proteins may play a role in transactivating many of the same downstream targets as those regulated by p53.7 This initially had lent support to the idea that perhaps these isoforms would be useful in re-activating targets of p53 in cancer cells (wherein the majority of cases p53 is either deleted or damaged). While a few of the isoforms of the proteins are overexpressed in several types of cancer, these have become the target of gene therapy and chemotherapy in order to attempt to have the active isoforms transactivate p53 downstream targets and suppress the tumor.
Current Approaches
Cancer is a very complex disease, and requires a broad and interdisciplinary approach to study it. The numerous research methodologies employed in cancer research are similarly diverse, and can be difficult to understand. However, over the last few decades, improvements in technology and advances in our understanding of genetics and proteomics had contributed significantly to our treatment approach to all types of cancer. The National Institute of Health has dedicated an additional $500 million over the last four years in order to investigate not only new treatment strategies for attacking cancer on a variety of fronts, but also to improve imaging and diagnosis.6 Traditional treatment for cancer involves surgery, followed by chemotherapy or radiation treatment. However, this approach does not ensure elimination of all cancerous cells. Thus, these traditional treatments cannot always prevent recurrence of tumors, which results in a poor long-term prognosis for the patient.
Fortunately, with the abundance of research over the last few decades, a variety of new therapies show promise. Several treatments are based on cancer biochemistry, which target key steps biological pathways to halt cell growth. Other treatments such as the Provenge® vaccine has shown promise in using the body’s own natural immune system to mount an effective response against cancer cells in the prostate.7 These types of cancer therapies differ from biochemically based treatments in that they do not attempt to fix or prevent cancer’s mechanism of growth. Immunotherapies use the body’s natural defense mechanisms to treat the cancer more as if it were a foreign pathogen.
In addition to directly treating cancer, there have been recent technological developments that have impacted cancer research. Use of technologies such as DNA microarrays and the recent completion of the Genome Project have helped researchers pinpoint genes implicit in the development of cancer. Novel imaging strategies, such as one used by physicians at Vancouver general hospital, utilize a new technology that fuses ultrasound and MRI to help screen patients for prostate cancer.9 Abstract mathematics has also been employed to study cancer. Dr. Roman Polyak has been instrumental in developing the theoretical framework for a mathematics-based approach to studying cancer. Recently, German physicians Dr. Alber and Reemtsen have applied his theory to “determine angle, intensity and duration for radiation beams to most effectively destroy cancerous tumors without damaging nearby healthy tissue.”10
New technologies and breakthroughs in biomedical research have the potential to generate more effective treatment strategies for cancer. Despite the seemingly disparate approaches taken to studying cancer, every new experiment and methodology sheds new light on the elusive mechanisms underlying cancer. With patience, ingenuity, and a bit of serendipity, cancer research may one day ensure that we never have to worry about weeds in our bodies again.
References
1Lewontin et al. (2003). n [Radio series episode]. In Big Ideas. n: ABC Radio National.
2 Mutation and Cancer. (n.d.). CancerQuest | A Cancer Education Resource. Retrieved January 2, 2011, from http://www.cancerquest.org/index.cfm?page=302
3 Gene mutations that can lead to cancer. (2009, July 8). Learn About Cancer. Retrieved January 2, 2011, from http://www.cancer.org/Cancer/CancerCauses/GeneticsandCancer/OncogenesandTumorSuppressorGenes/oncogenes-tumor-suppressor-genes-and-cancer-mutations-and-cancer
4 Levine, A. (1997). p53, the Cellular Gatekeeper for Growth and Division. Cell, 88, 323-331.
5 Levrero, M., Laurenzi, V. D., Costanzo, A., Gong, J., Wang, J., & Melino, G. (2000). The p53/p63/p73 family of transcription factors: overlapping and distinct functions. Journal of Cell Science, 113(10), 1661-1670.
6 Estimates of Funding for Various Research, Condition, and Disease Categories (RCDC). (2010, February 1). NIH Research Portfolio Online Reporting Tools (RePORT). Retrieved January 2, 2011, from http://report.nih.gov/rcdc/categories/
7 Small, E. J., Schellhammer, P. F., Higano, C. S., Redfern, C. H., Nemunaitis, J. J., Valone, F. H., et al. (2006). Placebo-Controlled Phase III Trial of Immunologic Therapy with Sipuleucel-T (APC8015) in Patients with Metastatic, Asymptomatic Hormone Refractory Prostate Cancer.Journal of clinical oncology,24(19), 3089-3094.
8 QM, G. (2003). DNA microarray and cancer. Current Opinion in Oncology, 15(1), 36-43.
9 Crawford, T. (2010, October 2). ‘Groundbreaking’ new technology eases diagnosis of prostate cancer. Vancouver Sun. Retrieved January 4, 2011, from http://www.vancouversun.com/health/Groundbreaking+technology+eases+diagnosis+prostate+cancer/3606185/story.html
10Rich, C. K. (2008, February 22). Using Abstract Math to Treat Cancer | LiveScience. LiveScience. Retrieved January 4, 2011, from http://www.livescience.com/technology/080222-bts-polyak.html
1 comment
Cool!!!!