Mission & Goals
The Partnership for Global Health Technologies aims to make an impact on healthcare delivery in developing countries while introducing students to the field of global health engineering. Through designing and developing context-relevant solutions in collaboration with local experts, the program provides students the opportunity to better understand the complex challenges facing many low-income countries and to craft inventive solutions to address those challenges. Our student researchers – comprised of undergraduates from Boston University and students from premiere educational institutions in Tanzania – share a passion for improving the health of families in resource-limited settings and is dedicated to reducing health disparities across the globe. Through combining the unique skill sets and perspectives of our diverse team, the Partnership for Global Health Technologies is constructing creative solutions to the world’s most serious health problems, and has become a model for experiential-learning engineering programs in the global health sphere.
Mission
The Partnership for Global Health Technologies strives to:
- Create affordable and marketable global health technologies in close collaboration with Tanzanian healthcare experts to ensure the local context is taken into account during the development process
- Foster a work environment that supports innovative and resourceful thinking among our student researchers
- Provide students with a comprehensive experience – from lab to bedside – in medical technology development
- Create the next generation of global health engineers who tackle the pressing health challenges facing our world
Goals
To improve bedside diagnostics for maternal monitoring and care
Each day, over 800 women die due to complications in pregnancy and childbirth globally.1 Over the past 25 years, development efforts have reduced the number of maternal deaths by 43%.1 Still, maternal mortality continues to be a pressing public health issue, perhaps nowhere more so than Sub-Saharan Africa, where more than half of all maternal deaths occur.1 These deaths are most often due to complications that are preventable or easily treated in developed nations.
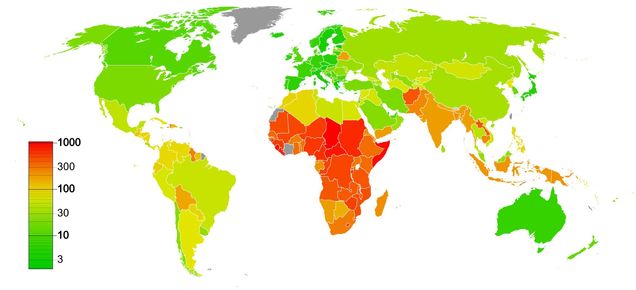
Zanzibar (the Republic of Tanzania) is one such example of a place struggling to reduce maternal and neonatal deaths. Maternal mortality rates in Zanzibar are over five times the Sustainable Development Goals’ 2030 target of 70 deaths per 100,000 live births.1 While Zanzibari maternal and child health indicators are better than those of mainland Tanzania, they are considerably higher than nearby South Africa and the United States.

The Partnership for Global Health Technologies wants to reduce this disparity by applying engineering and public health principles to maternal global health problems. While in Tanzania, we were routinely told about the difficulty of monitoring complications stemming from pre-eclampsia, a hypertensive condition that is associated with 10 – 15% of maternal deaths worldwide.4 We heard from a number of healthcare workers that there were no simple and quantitative tools to assess renal and hepatic health in pre-eclampsia patients rapidly at the beside, and that the diagnostic lab was often overburdened and under-equipped. In response, our team of student researchers is designing a bedside diagnostic that can monitor liver and kidney function, abilities that are often impaired in pre-eclamptic women. This paper-based technology would provide clinicians with quantitative results at a low cost, helping them to make better decisions in a timelier manner.
To ensure the quality of malaria rapid diagnostic at point of care
Rapid tests have greatly improved the way in which malaria is diagnosed. Instead of relying on a health facility to have the proper equipment and trained pathologists, and making the patient to wait for hours for a diagnosis, malaria rapid tests provide patients with a diagnosis in just minutes. However, there have been concerns over the quality of malaria rapid tests and the validity of their results, which could lead to the ineffective treatment of severely ill patients.5-8 Misdiagnosis of malaria also holds serious public health implications, as inappropriate use of antimalarials has been a leading cause in the emergence of drug resistant malarial strains across the world.

The Partnership for Global Health Technologies wants to provide a reliable, non-destructive and context-relevant method for quality assurance of malaria rapid tests that will allow clinicians to determine diagnostic quality at the point of care. With the use of a mobile phone camera, student researchers are working to determine whether physical differences can be detected between the images of functional and non-functional rapid diagnostics before and after use. We hope to design a mobile-based tool that clinicians can use to assess the quality of the rapid test before use and identify batches of poor quality tests, empowering local healthcare staff and improving the health of patients in malaria-endemic regions.
To create a dynamic systems model that will help hospitals reduce maternal mortality
Poor quality maternity care is becoming a major contributor to overall maternal mortality as an increasing number of women are persuaded to give births at health facilities. Barriers to adequate care during the ‘last mile’ of healthcare delivery are the result of deficiencies at multiple levels: education, staff, medication, facilities, delay in access to care. The contribution of each factor is difficult to ascertain in settings where even basic data registration is lacking. It is, however, crucial to try to unravel each factor’s impact on clinical outcomes because, with limited financial resources available, “more of everything” is not a viable strategy. With most of maternal mortality being preventable, a woman is likely to die because at one or several levels, the healthcare system in which she found herself failed her.

Our goal is to model the impact of policy changes at facility level on maternal mortality using a systems level approach. A decision aid that incorporates key parameters of the facility such as patient condition, severity of the case, and material and human resources will eventually guide policy-makers by providing insight on current determinants of maternal mortality and expected impact of policy changes. Our model can be used by administrators and procurement offices as a tool to make operational decisions at the facility level, ensuring the hospital or clinic is making the best use of their limited resources as they possibly can.
- Say, Lale et al. Global causes of maternal death: a WHO systematic analysis. The Lancet Global Health, Vol 2, Issue 6, e323-e333.
- UNICEF, 2010. Children and Women in Tanzania, Volume 2: Zanzibar.
- The World Bank, 2015. Maternal mortality ratio (per 100,000 live births) and neonatal mortality rate (per 1,000 live births).
- Duley, L. The global impact of pre-eclampsia and eclampsia. Semin Perinatol. 2009 Jun; 33 (3): 130 – 7.
- Harvey, Steven A. et al. Quality issues with malaria rapid diagnostic test accessories and buffer packaging: findings from a 5-country private sector project in Africa. Malar J. 2017: 160.
- Nankabirwa J, Zurovac D, Njogu JN, Rwakimari JB, Counihan H, Snow RW, et al. Malaria misdiagnosis in Uganda – implications for policy change. Malar J. 2009;8:66.
- Allen LK, Hatfield JM, DeVetten G, Ho JC, Manyama M. Reducing malaria misdiagnosis: the importance of correctly interpreting Paracheck Pf® “faint test bands” in a low transmission area of Tanzania. BMC Infect Dis. 2011;11:308.
- Laurent A, Schellenberg J, Shirima K, Ketende SC, Alonso PL, Mshinda H, et al. Performance of HRP-2 based rapid diagnostic test for malaria and its variation with age in an area of intense malaria transmission in southern Tanzania. Malar J. 2010;9:294.
- Nguyen Mai Huong, Sean Hewitt, Timothy M.E. Davis, Le Duc Dao, Tran Quoc Toan, Tran Bach Kim, Nguyen Thi Hanh, Vo Nhu Phuong, Doan Hanh Nhan, Le Dinh Cong; Resistance of Plasmodium falciparum to antimalarial drugs in a highly endemic area of southern Viet Nam: a study in vivo and in vitro, Transactions of The Royal Society of Tropical Medicine and Hygiene, Volume 95, Issue 3, 1 June 2001, Pages 325–329
