President Biden Is Being Treated for Sleep Apnea. How Common and How Dangerous Is the Condition?
BU sleep expert Sanford Auerbach explains its prevalence, risk factors, and treatment options
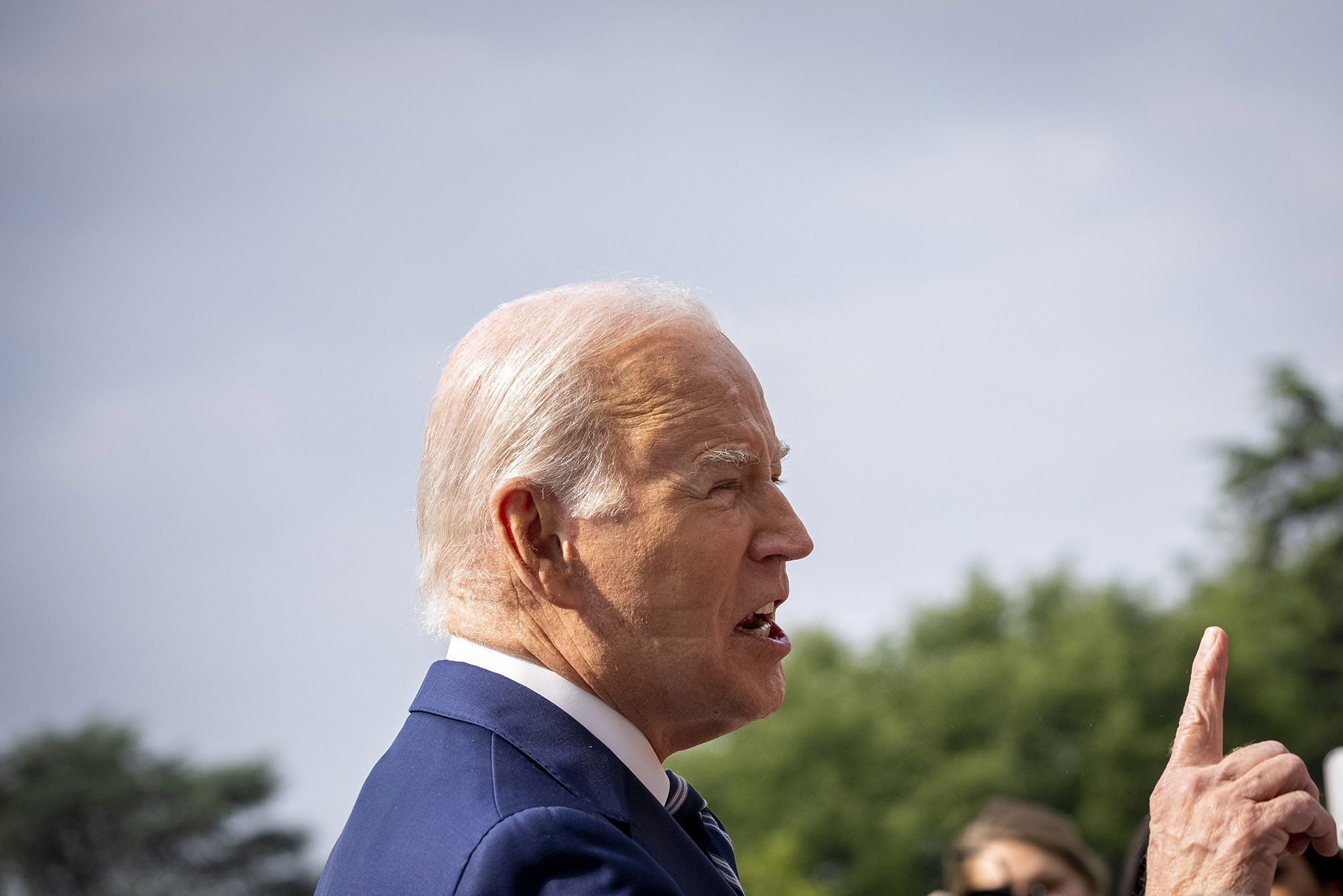
The White House announced on June 28 that President Biden, here speaking with members of the media, has started using a CPAP (continuous positive airway pressure) machine at night to help with sleep apnea. The announcement was made after indents from the mask were visible on the president’s face. AP Photo/Andrew Harnik
President Biden Is Being Treated for Sleep Apnea. How Common and How Dangerous Is the Condition?
BU sleep expert Sanford Auerbach explains its prevalence, risk factors, and treatment options
Last week, the White House announced that President Biden was using a CPAP—continuous positive airway pressure—machine to treat his long-standing sleep apnea, a common disorder that affects an estimated 30 million Americans. The revelation came after Biden, now 80, appeared in public with indentations on both sides of his face caused by the straps used to hold the machine’s air pressure mask in place.
Those with the disorder have disruptions in their breathing when they are asleep. This can lead to inefficient sleep and restriction in the normal flow of oxygen to the brain. Obstructive sleep apnea (OSA)—the most common form of the disorder and the one that President Biden has—occurs when the airway collapses while a person is sleeping, causing a reduction in the airway. Left untreated, sleep apnea can have serious health consequences. One of the most common ways to treat it is with a CPAP machine, which delivers a steady stream of air pressure through a mask, helping to keep breathing passages open.
To find out more about sleep apnea and treatment options, BU Today reached out to Sanford Auerbach, an associate professor of neurology and psychiatry at Boston University’s Chobanian & Avedisian School of Medicine. Auerbach is a board-certified sleep specialist and director of Boston Medical Center’s Sleep Disorders Center. He spoke with us about the symptoms to look out for, what can be done to reduce your risk of developing the disorder, and how CPAP machines work.
This interview has been edited for length and clarity.
Q&A
with Sanford Auerbach
BU Today: What are the risk factors for developing sleep apnea?
Auerbach: Risk factors include age, obesity, gender—males are more likely to experience sleep apnea than women—snoring, high blood pressure, diabetes, anatomy, and evening alcohol consumption.
BU Today: So President Biden’s age and gender increased his risk of developing the disorder?
Auerbach: Yes. It should be noted, however, that we see young, thin women with OSA [obstructive sleep apnea].
BU Today: Sleep apnea is widely believed to be underreported, with many people not knowing they have it. What are the symptoms?
Auerbach: The typical patient may present with a history of loud snoring, disruptive sleep, observed disruptions in breathing during sleep, concentration and memory complaints, and daytime fatigue and/or sleepiness. There are also other symptoms that may be associated. These include forgetfulness, concentration problems, increased need to urinate through the night, and irritability.
BU Today: How is it treated?
Auerbach: CPAP is commonly used. Other options for selected patients include weight loss, attention to body position (for example, sleeping on one’s back may make it worse), oral appliances, and certain surgeries, usually performed by an ENT specialist or an oral surgeon. There is also a relatively new approach that involves electrical stimulation of the nerve to the tongue that will cause the tongue to move forward during sleep and allow for an increase in the airway. There are other options that are available, too.

BU Today: How does a CPAP machine work and how does it help promote better sleep?
There is a mask worn over the face. It is hooked up to a small air compressor and the unit delivers compressed room air. This is sufficient to keep the airway open. The pressure is low enough so that the patient can easily breathe in and out. Breathing improves, sleep quality improves, and it usually eliminates snoring. Patients should feel better during the day.
BU Today: Is there a cure for the disorder?
In most cases, it’s a matter of treatment. In some cases, there can be a cure with surgery. Some overweight patients may eliminate the problem with weight loss. Obesity is a common risk factor. But otherwise it’s a matter of treatment and CPAP is considered the gold standard.
BU Today: Are there dangers if sleep apnea goes untreated?
If untreated, obstructive sleep apnea can lead to daytime symptoms including fatigue, sleepiness, and problems with concentration. It is also thought to contribute to the risk of cardiovascular and cerebrovascular disease. There is reason to suspect that if untreated, it can contribute to cognitive impairment and even dementia in the elderly.

Comments & Discussion
Boston University moderates comments to facilitate an informed, substantive, civil conversation. Abusive, profane, self-promotional, misleading, incoherent or off-topic comments will be rejected. Moderators are staffed during regular business hours (EST) and can only accept comments written in English. Statistics or facts must include a citation or a link to the citation.