BU Publishes Public Health Data from Its Fall 2020 COVID Surveillance Efforts
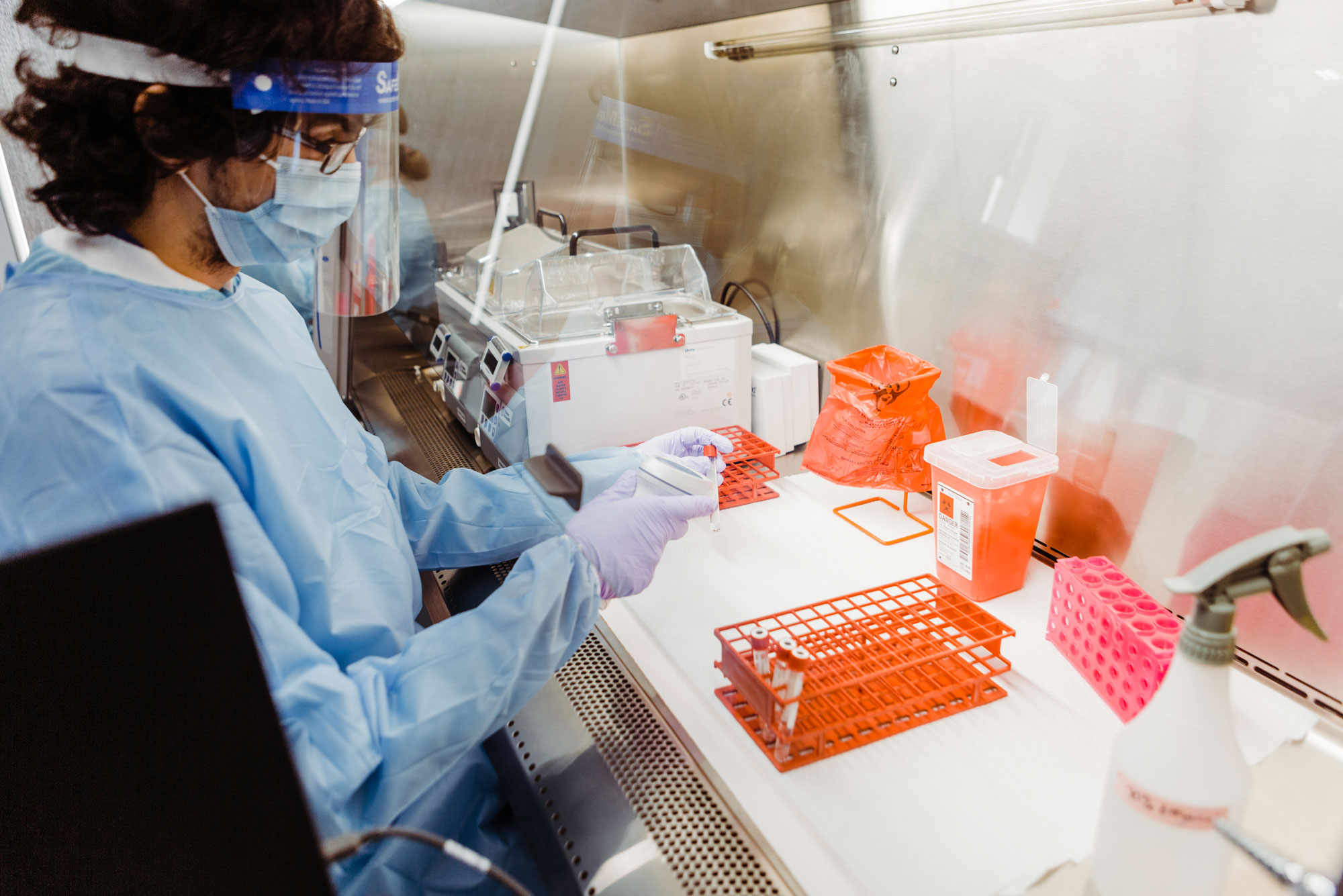
Each week, BU’s Clinical Testing Lab processes roughly 30,000 coronavirus tests from asymptomatic BU students, faculty, and staff. Photo by Janice Checchio
BU Publishes Public Health Data from Its Fall 2020 COVID Surveillance Efforts
University leadership and scientists, in detailed case study of COVID-related measures and outcomes, hope BU’s insights can aid other institutions, corporations
Editor’s note: On June 25, 2021, these case study results were published in the peer-reviewed journal JAMA Network Open.
Living, working, and learning amidst a constant viral threat: Boston University leaders and scientists have written a case study documenting the lengths it took to safely reopen a residential university in one of the country’s most bustling urban centers. The case study, published today as a preprint paper on medRxiv, stands as a testament for what’s possible in our new normal of living in the COVID-19 pandemic era, and as a potential roadmap for other institutions and corporations, weary of remote functioning, that seek a path to bring people back together in person.
In March 2020, as the coronavirus pandemic began to boil over in the greater Boston area and throughout the United States, BU leadership asked the majority of its 40,000-person community—students, faculty, and the vast majority of staff and researchers—to leave campus, with no idea when they’d return. Within a few weeks, it became clear that the pandemic surge was only getting worse, and scientists at the National Emerging Infectious Diseases Laboratories (NEIDL) and BU’s Schools of Medicine and Public Health forecasted that life would not return to normal anytime soon, perhaps a year or more.
Almost as soon as BU closed its doors, University leadership began building coronavirus response teams of its own—educators, scientists, engineers, clinicians, and laboratory technicians.

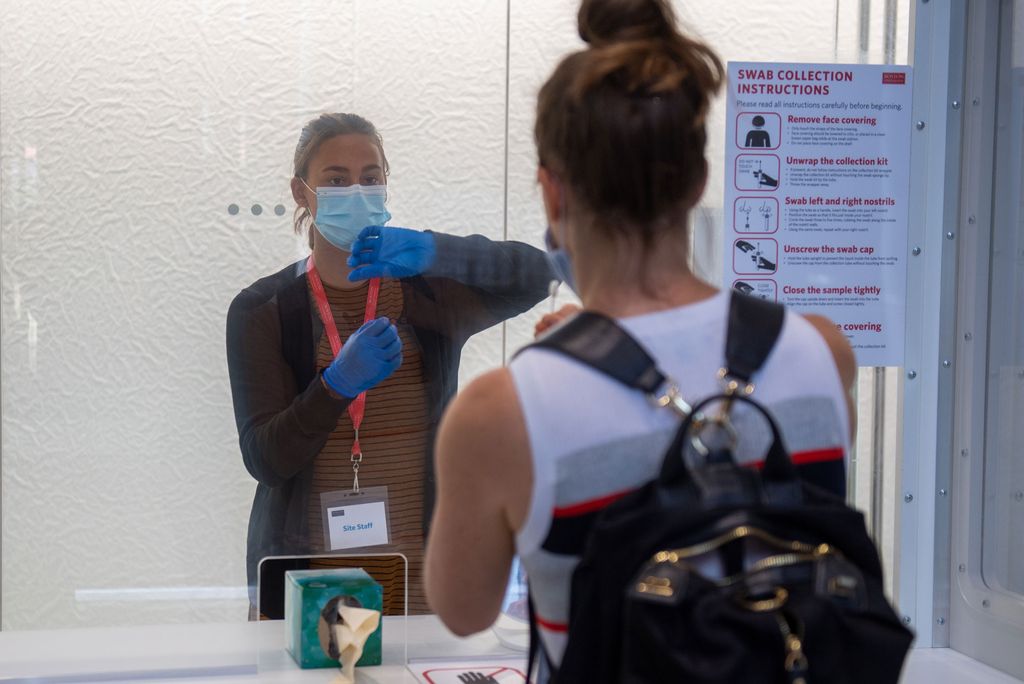
Photo courtesy of the BU Office of the Provost
“There was buy-in from BU leadership from the start,” says Gloria Waters, BU’s vice president and associate provost for research and a coauthor on the case study. “[BU President Robert Brown] is an engineer. He wanted BU to develop solutions.”
BU’s COVID response task forces faced the massive undertaking, over the course of spring and summer 2020, to figure out a way to reopen BU’s urban campuses amidst a raging global pandemic.
They implemented a hybrid learning model, called Learn from Anywhere, that would allow remote and in-person curriculum to blend as seamlessly as possible. They designed a computer simulation of BU’s campus and community, modeling how the virus might spread through BU’s network of people and testing out the impact of various proposed intervention strategies, should in-person classes and work resume. Then, bolstered by what the model predicted, they put a reopening plan into action.
They set up nasal swab sampling sites around BU and developed a digital appointment tool to keep foot traffic to the sampling sites spaced out in an orderly fashion. They built out lab space and purchased new machinery to create a clinical testing lab capable of screening thousands of tests per day for SARS-CoV-2, the virus responsible for COVID-19 infections. And they hired technicians who would keep those machines humming 12 hours a day, 7 days a week.
BU hired and trained contact tracers who would work tirelessly to identify and isolate close contacts of people at BU who had tested positive for coronavirus. And they set up designated quarantine housing and isolation housing, a total of 650 and 342 units, respectively, to separate and care for students who had been exposed or infected with coronavirus.
At the start of the fall 2020 semester, BU reopened its doors to residential learning, a meticulously thought-out experiment in how University life could go on in spite of coronavirus. The decision did not come without criticism, notably from some faculty and staff members who felt that any resumption of in-person classes would put them at risk, and that in reopening, BU was choosing its financial health over the well-being of its community.
The reopening plan itself came with a high financial cost, the BU case study authors say. “BU had to implement budget adjustments, including hiring freezes, salary freezes, and several other cost-cutting measures to meet the cost of these services and respond to declining revenue because of pandemic-related changes to operations,” they write. Despite a difficult decision to make a few hundred layoffs and furloughs, overall “the university was able to meet its financial obligations and avoid large layoffs or other consequential financial impacts in the fall.”
And the goal to prevent coronavirus from spreading amongst BU’s reopened campus was, largely, successful. On top of all the regular testing, public health protocols, contact tracing, and other measures, BU’s leadership relied on real-time data for “nimble decision-making” in response to new infections that cropped up on campus. In the case study, the authors further detail the results of BU’s fall 2020 semester.
COVID on campus, by the numbers
Between August and December 2020, the newly minted BU Clinical Testing Lab processed over half a million COVID-19 tests, collected from five sampling sites sprinkled across BU’s Charles River and Medical Campuses. From those tests, a total of 719 individuals—about 1.8 percent of BU’s coronavirus testing population—tested positive for coronavirus over the course of the fall semester: 496 students, 11 faculty, and 212 staff. Nearly 38 percent of all positive cases were asymptomatic, and likely would have gone undetected without BU’s rigorous testing regime.
BU’s contact tracing team identified 837 people who had been in close contact with people who had tested positive. Of those close contacts, 10.3 percent of them went on to test positive for COVID-19 within the quarantine window.

Photo by Cydney Scott
“Contact tracing is key,” says Davidson Hamer, a member of BU’s Medical Advisory Group and a faculty member at BU’s Schools of Public Health and Medicine, and at the NEIDL. Throughout the pandemic, he’s provided guidance to the Massachusetts higher education reopening task force, and he chairs a group where clinicians and leaders from BU, Harvard University, Tufts University, Massachusetts Institute of Technology, and Northeastern University share data and insights on campus coronavirus response efforts.
“The data shows that BU’s contact tracers were identifying and getting in touch with potentially exposed close contacts within hours of an individual testing positive for COVID-19,” Hamer says. On average, close contacts were notified of potential exposure within 6.4 hours of someone testing positive for COVID-19. BU’s Clinical Testing Lab also kept a rapid pace, averaging a 12- to 15-hour turnaround time after an initial and expected learning curve and ramp-up period at the semester’s beginning. “Relative to the speed of COVID-19 transmission, when it comes to testing and tracing speed, we nailed our objectives.”
BU also enforced public health measures to aid in reducing transmission: mask use, social distancing recommendations, enhancing all building air systems, requiring digital daily health attestations for anyone approved to visit campus, and de-densifying the number of people in classrooms, laboratories, and office spaces.

Photo by Cydney Scott
“Most classes had around 20 percent of students reporting that they planned to attend classes in person; that’s a big de-densification,” says Eric Kolaczyk, a statistician and the director of BU’s Rafik B. Hariri Institute for Computing and Computational Science & Engineering. He coordinated the BU team that developed and now maintains operation of BU’s computer simulation of its campuses and community.
BU’s contact tracing team didn’t discover any case clusters or transmission of COVID-19 cases linked to on-campus classes. Instead, they discovered that the majority of spread within BU’s community occurred off campus—which at times was associated with a twice as high probability of testing positive for coronavirus compared to on-campus students—either at non-University-sanctioned gatherings or exposure to the surrounding Boston community. At one point during the semester, BU’s off-campus community lagged significantly in complying with BU’s regular testing cadence, although those numbers eventually improved.
Contact tracers identified a definitive source of transmission in about half of all positive cases. Of those sources, 55.7 percent came from outside of the BU community. Among faculty and staff whose infection could be linked to a specific source, non-BU sources of infection were identified 100 percent and 79.8 percent of the time, respectively.
A total of 7,266 graduate students (99 percent) lived off campus. In contrast, most undergraduates (67 percent) opted to live on campus in BU housing, a total of 7,131 students. Of those on-campus undergraduate residents, 3,453 (48 percent) lived alone and 3,678 (52 percent) lived with one roommate. These unusually small on-campus household sizes were the direct result of BU’s de-densification measures. BU household contacts were identified as a source of transmission in less than 1 percent of cases.

The contact tracing team encountered challenges, however, when some students were reluctant to “divulge information regarding where they had been or who they had been with,” the case study authors write.
Over time, BU’s rate of new cases per 1,000 people remained similar to the Suffolk County curve, although because Suffolk County residents were not undergoing regular asymptomatic testing like BU’s community was, BU was able to identify rising COVID-19 rates earlier.
The most notable COVID-19 spikes at BU and around Suffolk County followed on the heels of holidays, including the three-day Indigenous Peoples’ Day weekend, Halloween weekend, and Thanksgiving week.
Learning from lived experience, captured by data science
“That’s a lesson for us to remember this spring and summer; when you have a holiday or a long weekend, you have gatherings,” Hamer says. “And within three to five days of those gatherings, if you’re doing asymptomatic screening like BU, you can start to see COVID-19 cases increase. We’ve got to restrict our gatherings with other households, that’s a very important message.”
The biggest increase in COVID-19 cases followed Thanksgiving; at BU, the spike of new cases was more prevalent in undergraduate students and non-faculty staff.
“If you employ multiple interventions with great adherence to those policies”—masking, distancing, de-densification, routine symptom attestation and testing—“you can greatly limit the spread of COVID-19, even without vaccines,” Hamer says. “Since our campus is mixed into the city of Boston, it’s hard to escape what’s happening in the community, but with strict public health measures and enforcement, we were able to keep the spread of coronavirus under control.”
Kolaczyk says the learnings from BU’s fall 2020, predicted by his team’s sophisticated computer simulation modeling BU’s community behavior, are in many ways not surprising given what we know from history’s earlier pandemics.
“In some sense, we knew what public health measures worked 100 years ago,” Hamer says. “If you compare our interventions back to the ones used in 1918 [during the Spanish influenza pandemic], back then people were closing public spaces, wearing masks, distancing from other people, opening up their windows to increase airflow and ventilation. But back then, they didn’t have the added benefits of testing or contact tracing.”
Today, Hamer says, BU can thank data systems for the success of fall 2020.
“Software [developed by BU IS&T] to propagate testing, symptom attestation, residence, and classroom information into a data-driven dashboard allowed BU’s leadership and Medical Advisory Group to do fairly quick interventions as infections sprung up on campus,” Kolaczyk says. “At the very essence, computing and data science have given us actionable insights.”
Kolaczyk says that BU’s large size and location in Boston’s urban environment gave it a unique challenge in terms of reopening safely. But those same factors—the breadth and depth of its faculty experts who are part of Boston’s premier scientific and medical fabric—are what ultimately made BU’s reopening plan and COVID surveillance program possible. “BU has a huge amount of resources in terms of human expertise—there were a lot of slices of academia that came together to pull this off,” he says.
“I’m an epidemiologist and Eric is a mathematician, we’d never even met before the pandemic hit,” Hamer says. “BU’s infrastructure played an important role in this—for leadership to buy into a reopening plan, for BU to have the right financial resources, and most importantly, for BU’s intellectual resources to bring together the right expertise.”
Waters agrees. And she says BU’s COVID surveillance program will make especially important contributions to public health data now that COVID variants and vaccines have entered the landscape of the pandemic. BU is now taking the additional step of sequencing the genetic signature of all positive COVID samples, collecting new information that could explain how coronavirus is changing over time, and how those changes impact the way the virus spreads.
“One thing that’s really unique to BU is that infectious disease is one of our areas of excellence—we have the NEIDL, and this is precisely the type of work that lab was built for,” Waters says. The variant sequencing data from the NEIDL will not only give BU clarity on what strains are circulating in its campus community, but that information will also be shared with public health officials from the city of Boston and the state of Massachusetts to aid in their mission to better understand how COVID is impacting communities in the region.
Waters says that BU’s COVID surveillance program may also help answer some of the questions still remaining about the new COVID vaccines; how effective they are, how long immunity lasts, and whether people who have been vaccinated can still transmit the virus to others.
“In the clinical trials for the COVID vaccines, those participants were not undergoing asymptomatic COVID screening, so there are still a lot of open questions about whether people who have been vaccinated can spread the virus,” Waters says. “The sooner we can create a dataset around that, the better—at BU, we’re doing 30,000 tests per week on asymptomatic people, so as more people get vaccinated, we’re going to gain a wealth of data that few other places are able to collect. If we can find out that people who have been vaccinated are not asymptomatic carriers of the virus, that knowledge will help the world open back up again more quickly.”
Editor’s note: This story was updated on March 1 to reflect a mathematical correction made in the case study. The case study had originally reported 627 students tested positive for coronavirus during the fall 2020 semester. The correct number is 496 students.

Comments & Discussion
Boston University moderates comments to facilitate an informed, substantive, civil conversation. Abusive, profane, self-promotional, misleading, incoherent or off-topic comments will be rejected. Moderators are staffed during regular business hours (EST) and can only accept comments written in English. Statistics or facts must include a citation or a link to the citation.