How Light Turns Ordinary Hydrogen Peroxide into a MRSA Treatment
BU engineers have invented a new blue light therapy that can kill MRSA without antibiotics
As a kid, I skinned my knees on a range of surfaces, from our asphalt driveway, to wood chips on the playground, to the concrete deck of our town pool. I usually cried, not because of the fall itself, but because I knew any scrape deep enough to bleed would attract the attention of my parents and cause them to reach into the medicine cabinet for that dreaded bottle of hydrogen peroxide. Oh, the stinging!
But now, a few decades later, I’ve finally found a reason to appreciate hydrogen peroxide. It turns out that it’s powerful enough to kill a particularly lethal kind of antibiotic-resistant bacteria—as long as it’s combined with a blue LED light or laser.
Boston University College of Engineering researchers who invented the technique say they have shown, experimentally, it can kill 99.9 percent of methicillin-resistant Staphylococcus aureus, known as MRSA. (Methicillin is a common antibiotic.) In people, MRSA, which often spreads very quickly, can cause skin and soft tissue infections as well as life-threatening sepsis.
Ji-Xin Cheng, the senior author on the Advanced Science paper about their findings, says it was a Boston University CARB-X report that inspired a few members of his biophotonics lab—which manipulates the properties of light for biological and medical applications—to join the fight against antibiotic resistance. The CARB-X report indicated that antibiotic development cannot keep pace with evolving bacteria, and that nonconventional approaches are needed, says Cheng, who is a professor of biomedical engineering and electrical and computer engineering.
“Can we use photons to deal with superbugs?” he asked his team.
Shining a light on superbugs
Cheng’s lab was most interested in tackling MRSA, since it’s difficult to treat and can cause deadly pneumonia infections and sepsis. MRSA infections affect about 90,000 people each year in the US, and cause around 20,000 of those people to die. Although MRSA can thrive any place where people come into contact with each other—from a supermarket to a school to an office—it’s especially common in hospitals and nursing homes, where people are more likely to have surgical incisions and skin abrasions. Opportunistic MRSA infections often take root in small breaks in the skin, but because antibiotics aren’t very effective in treating them, can quickly spread throughout the body.
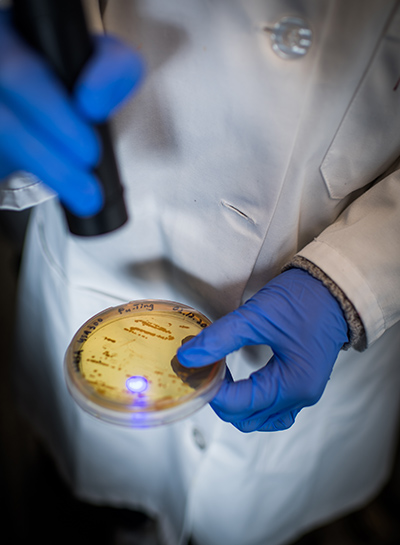
While taking a closer look at MRSA in their lab, Cheng’s team realized that MRSA’s signature golden color could be the golden ticket to a powerful new treatment.
“Golden pigmentation is the universal signature of S. aureus,” he says. While imaging S. aureus under the microscope, the team noticed that blue light caused a traumatic photobleaching effect—destroying pigment molecules responsible for the cells’ golden color—in as fast as seconds of exposure. “For imaging purposes, this is bad,” Cheng says. “But if it’s bleached, we wondered, is it still alive?”
When MRSA’s golden pigment molecules decompose under blue light, the cell membranes become checkered with vulnerable spots, says Pu-Ting Dong, the lead author on the study. The team found that blue light destabilizes MRSA cells enough to kill about 90 percent of the bacterial culture. That sounds powerful, but for clinical applications, Dong says, 90 percent isn’t good enough. In fact, in as little as half an hour, the researchers observed that MRSA was able to recover and start to multiply again. “MRSA grows back very quickly, so to be effective,” Dong says, “we need to kill 99.9 percent of bacteria.”
What could kill that last, critical 10 percent of MRSA cells? Hydrogen peroxide—a powerful oxidizer that can damage living cells.
A “photon” finish for MRSA
Typically, MRSA and other types of cells are able to withstand being doused with hydrogen peroxide through the defenses of their cell membranes. But after blue light phototherapy, MRSA’s membranes become temporarily pockmarked with holes. When hydrogen peroxide is delivered in combination with blue light, it’s able to flood the insides of MRSA cells and cause them to biologically implode, eradicating 99.9 percent of bacteria.
“Antibiotics alone cannot effectively get inside MRSA cells,” Cheng says. “But photons can penetrate a cell,” giving a window of opportunity for hydrogen peroxide to wreak havoc.

Perhaps what’s most promising is that blue light phototherapy doesn’t affect healthy cells of the body, so the technique could be used to treat MRSA infections without harming any surrounding tissue or skin.
Although the tests in culture dishes were exciting, biochemistry is always a little different in living organisms. Partnering with Purdue University microbiologists and researchers at the Massachusetts General Hospital Wellman Center for Photomedicine, the group analyzed the therapy’s effectiveness in mice and observed that the blue light plus hydrogen peroxide treatment was able to speed healing of skin wounds infected with MRSA.
Since then, the team has made further strides, discovering that pulse laser therapy is even more effective at killing MRSA.
“Using a pulsing blue laser, we can significantly shorten the therapy time and increase the depth of tissues we can effectively treat,” says Jie Hui, a postdoctoral researcher in Cheng’s lab and a coauthor on the paper. “The laser light feels painless and doesn’t give off any sensation of heat, ideal for clinical applications.”
Now, Cheng’s lab is teaming up with David Negron, a foot surgeon at Boston Medical Center and instructor of surgery at BU School of Medicine, to develop a clinical trial evaluating the technique’s ability to treat patients with diabetic ulcers.
“Diabetic skin ulcers are a huge problem,” Cheng says.
Having diabetes, which causes high blood sugar, can damage a person’s circulation and nerves, making it more difficult for the body to heal wounds, especially those located on the lower extremities. Open wounds that can’t heal are highly susceptible to MRSA, and until now, there haven’t been any good options for treatment. As the infection takes hold, it can create a biofilm, a slimy buildup of bacteria that becomes even more stubborn to treat.
“If we can treat diabetic ulcers, that will change people’s lives,” Cheng says. “As scientists, we don’t just want to publish papers, we also want to return the fruits of our work and research funding to society.”
Dong, who won an International Society of Optics and Photonics (SPIE) Translational Research Award for her work on this technology, says she personally feels “inspired and motivated” to translate the technique now that there’s a clear clinical application that “could help people heal.”
Hui’s work on the team has also been recognized; he was awarded the SPIE-Franz Hillenkamp Postdoctoral Fellowship, which will support him as he works to develop the phototherapy into a tool that can make MRSA vulnerable to conventional antibiotics.
This work was supported by a Keck Foundation Science & Engineering Grant and a Boston University start‐up fund.


Comments & Discussion
Boston University moderates comments to facilitate an informed, substantive, civil conversation. Abusive, profane, self-promotional, misleading, incoherent or off-topic comments will be rejected. Moderators are staffed during regular business hours (EST) and can only accept comments written in English. Statistics or facts must include a citation or a link to the citation.