Patient Navigators Improve Delivery of Care for Breast Cancer Patients
BMC program reduces cancer disparities by addressing barriers to timely care
Tracy Battaglia was an undergraduate at BU studying psychology in 1990 and planning to begin medical school at the School of Medicine, when she was diagnosed with stage 4 lymphoma. “I had a positive experience with my treatment and did not encounter any delays in my care,” says Battaglia (CAS’92, MED’96, SPH’01). After completing her residency, she returned to BU in 1999 for a fellowship in general internal medicine and women’s health, and started seeing patients who had just been given a cancer diagnosis—or a potential cancer diagnosis—and many of them weren’t coming back for care.
“There were things in their way, and that really resonated with me,” says Battaglia, now director of MED’s Women’s Health Unit: Center of Excellence in Women’s Health and a practicing clinician in the Women’s Health Group clinic at Boston Medical Center (BMC). She was bothered by the dichotomy she saw between the city’s vast medical resources and this vulnerable patient group. “Boston has an embarrassment of riches, and yet we still had a population that was delaying care,” she says, and then she asked herself, “Why was that the case and what could we do to treat that critical disconnect?”
12%
BMC’s patient navigation program demonstrated a 12% improvement in mammography screening rates.
Battaglia, a MED associate professor of medicine, a School of Public Health associate professor of epidemiology, and director of medical education at BMC’s Belkin Breast Health Center, was sure there were things that could be done to improve the problem. “We did focus groups and key informant interviews, and we tried to understand what the challenges were for patients to come in. We found many, including a lack of coordination of services,” she says. “The system was so fragmented that patients were confused, and they had their own specific barriers to navigating the system.” Those ranged from lack of transportation and insurance to language barriers and sociocultural issues that breed fear and mistrust.
Teaming up with the Avon Foundation in 2001, Battaglia helped launch what was one of the country’s first patient navigation programs, where underserved breast cancer patients are paired with a navigator from the same neighborhood, or one who shares similar culture or language, to help deal with the numerous issues that could block the patient from timely care.
BMC’s early patient navigation program—initially called care coordination—was developed on the heels of a similar program launched by Harlem Hospital surgical oncologist Harold Freeman in New York City in 1990. Freeman had seen that women in medically underserved or minority communities had greater barriers to screening, diagnosis, and treatment than those with better access to care. With patient navigators helping these women overcome obstacles to care, he found, their outcomes changed markedly. At Harlem Hospital alone, the five-year survival rate jumped from 39 percent prior at the program’s start to 70 percent. BMC’s patient navigation program targeting underserved and minority women in Boston demonstrated a 12 percent improvement in mammography screening rates and a 15 percent improvement in timely follow-up rates after an abnormal screening test and helped reduce missed appointments at BMC by 50 percent.
Bridge between patient and health care provider
Based on the strength of their early work and their collaboration with Freeman, Battaglia and BMC colleagues were selected to be part of the Patient Navigation Research Program (PNRP), a five-year, $25 million study funded by the National Cancer Institute that began in 2005. The study’s nine sites nationwide recruited vulnerable breast cancer patients to demonstrate the effects of patient navigation from the time of an abnormal screening through diagnosis and treatment.

The BMC contingent partnered with six federally qualified community health centers to implement navigation intervention for women with abnormal breast screening or new cancer diagnoses. In cooperation with an active community advisory board and a national steering committee, they worked to reduce delays in care by designing a rigorous scientific study of patient navigation that was focused on identifying and addressing the barriers patients faced. The Boston PNRP partnership enrolled more than 3,000 participants, 68 percent of them minorities.
Along with colleagues like BMC medical oncologist Naomi Ko, a MED assistant professor of hematology and medical oncology, Battaglia designed a program that had breast cancer patients deemed most at clinical risk meet with a navigator as soon as they arrive at BMC. The navigators, laypeople without professional degrees, but with some experience with the health care system, serve as a bridge between patient and health care provider, working one-on-one with patients to help coordinate care, making sure that they have transportation to appointments, helping them fill out forms for family and medical leave, and connecting them to additional services, like a food bank, when necessary.
Numerous rigorous studies conducted by Battaglia, Ko, and others at BU have confirmed that the program works. “We’ve demonstrated improvements in screening rates, we’ve demonstrated reductions in times of diagnosis, we’ve also demonstrated reductions in time of treatment,” Battaglia says. The PNRP is the largest national study to date of patient navigation, and its data clearly showed benefits in cancer care, with a greater proportion of patients beginning more timely care. It also documented a greater adherence to guideline-recommended cancer care for navigated patients and showed that navigation had the most benefit in patient populations with the greatest needs and longest delays in care. Specifically, the PNRP found groups of patients who had the greatest benefit from patient navigation: those who reported a greater number of barriers to care, and in particular, patients with social service barriers (those considered the social determinants of health), among them insurance, income, education, family stability, and safety, had the greatest benefits from navigation.
The PNRP data amassed so far suggest that patient navigation is an effective tool. Today, it is an expected standard at any hospital accredited by the American College of Surgeons Commission on Cancer. Seeing how effective BMC’s navigation program has been, numerous clinics in and around Boston have adopted similar ones.

Wanda Turner, senior patient navigator with the Avon Breast Health Initiative (left), with patient Franscheska Eliza at BMC’s Belkin Breast Health Center.
Not every patient seen at the Belkin Breast Health Center is paired with a navigator. “We use protocols to identify the highest risk patients by pairing patients who have abnormal imaging, are in need of a biopsy, have an increased risk of breast cancer due to genetic mutations or family history, and any patient for whom a provider has identified barriers that may interfere with timely care,” says Amy Fitzpatrick (MED’06), clinical supervisor of the Avon Navigation Program in the Belkin Center.
Battaglia says she and colleagues are continually refining their patient navigation program to make it more responsive. She and Ko are currently conducting a randomized controlled study, called Project Support, funded by the NGO nonprofit Patient-Centered Outcomes Research Institute (PCORI), to determine whether adding legal advocacy to patient navigation services at BMC will result in more timely care for women with newly diagnosed breast cancer. Preliminary studies have shown that sociolegal barriers—issues like housing, utilities, and legal status—reduce the effectiveness of patient navigation. “The more barriers present, the less timely a patient’s care,” Battaglia says.
The BMC team enlisted community members to help design the Project Support study, begun in 2013 and running through 2018. They created an advisory group of BMC cancer patients to help them write the grant application, and once they received funding, to help them decide how best to approach and recruit new patients. “They helped us pilot the surveys and refine them,” Battaglia says, “and they continue to meet with us every other month to give us feedback as we identify challenges in the program.”
The person who fixes things
Community outreach is critical to their success. “I’m a white woman, not of Boston, which sets up a level of distrust,” Battaglia notes. “A lot of researchers don’t want to take the time to cultivate that trust because it takes away from writing papers and doing studies, and it slows you down. But for me, it’s the most exciting part of the work.”
Team members work hard to engage the care providers, who are not necessarily researchers, and the public health agencies, like the Boston Public Health Commission and the Massachusetts Department of Public Health, providing community services to patients. While that kind of relationship-building takes an intensive amount of time and resources, it’s worth it, Battaglia says, “because we get solutions that will work and stick.”
There are currently four navigators working with breast cancer patients at BMC—one who works with women from the time they receive an abnormal screening up until diagnosis (that position has been funded by the Avon Foundation since 2001) and three who follow women from diagnosis through treatment. Those positions are funded by BMC and by research grants from PCORI and the American Cancer Society.
15%
BMC’s patient navigation program demonstrated a 15% improvement in timely follow-up rates after an abnormal screening test.
Wanda Turner, the senior patient navigator with the Avon Breast Health Initiative, is the first point of contact. When patients arrive, Turner meets with them to help identify any barriers that might prevent them from receiving timely care.
Turner, who is African American, says it’s important for patients to see someone they can identify with. “Patients feel more comfortable when talking to somebody they think looks like them,” she says. “I was born in Boston and raised here, and most of the population that comes here looks like me.”
Sometimes, her work involves just listening. If a patient has only recently been given a diagnosis of breast cancer, it can be overwhelming. “They’re not hearing anything that you’re saying to them. They don’t even remember what their provider looks like,” Turner says. She takes her lead from the patient: if they want to talk, she lets them talk. If they don’t, she simply assures them that she’ll be with them in the weeks and months ahead.
“Picture a woman who’s unemployed and homeless, a victim of domestic violence, and she’s had an abnormal mammogram. She needs further tests, but is so afraid to come in for the tests, plus she has insurance issues, she doesn’t know how to work the system, who to call. I’m kind of the person who fixes things,” says Turner. “I’ll say, ‘Let me call your insurance to see if we can see what’s going on.’ ‘Let me explain to you what the doctor just told you in a language you can understand, if that went over your head.’”
“Once patients leave the office, the navigator is their point of contact to get them back in,” says Battaglia. “The navigator will call them up if there are any outstanding issues, and is the liaison to the health provider.”
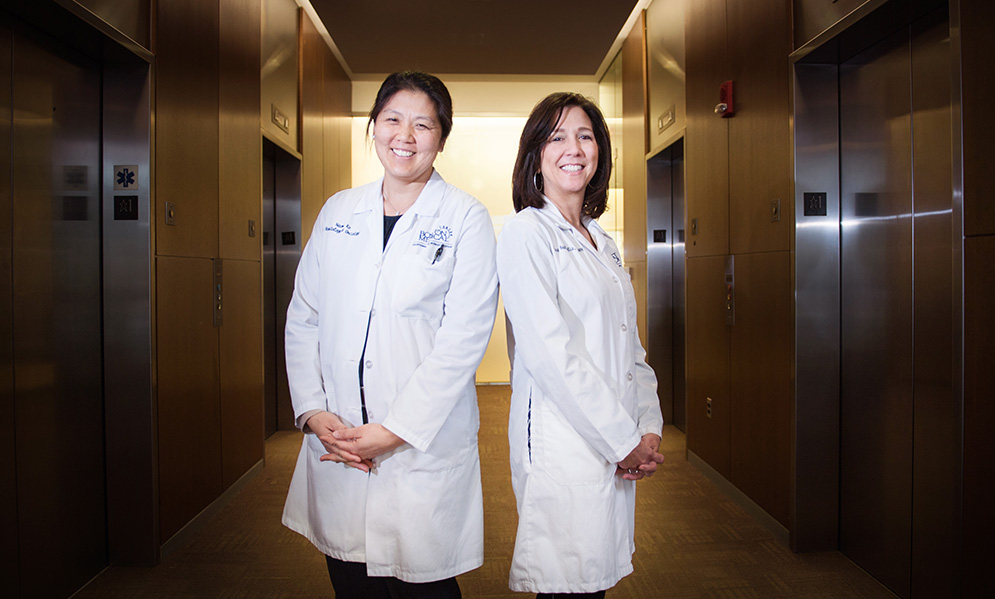
Tracy Battaglia (right), director of MED’s Women’s Health Unit: Center of Excellence In Women’s Health and director of medical education at BMC’s Belkin Breast Health Center, along with colleagues like Naomi Ko (left), a MED assistant professor of hematology and medical oncology, has conducted numerous rigorous clinical studies that show that patient navigation programs improve mammography screening rates and timely follow-up rates after an abnormal test screening for breast cancer.
BMC is the largest safety-net hospital in New England, and the need for such a program at a hospital like that is enormous. BMC treats approximately 200 newly diagnosed breast cancer patients each year. More than half of the hospital’s patients have an annual income of less than $20,000, nearly 70 percent are racial and/or ethnic minorities, and over 50 percent are on publicly insured health plans.
The problem of cancer disparities is already well documented, Ko says. “We know it’s a huge problem. You can cut the data every which way, and if you’re black, you’re going to do worse.” Statistics show that African American women with breast cancer are diagnosed at a younger age than white women, are 42 percent more likely to die from the disease than white women, and are at double the risk for developing triple-negative breast cancer, a particularly aggressive form of the disease, than white women. So improving care delivery, by inference, will improve survivorship.
50%
The patient navigation program helped reduce missed appointments at BMC by 50%.
There are many different ways to attack these disparities, says Ko. “There isn’t a single magic bullet.”
Turner is convinced that without the patient navigation program, those women unable to advocate for themselves “would fall through the cracks. They wouldn’t get the proper care,” she says. “If you can save just one person’s life or get them the care they need, you’ve done something at the end of the day.”
Despite the successes at BMC, there remains a citywide disparity in cancer care for minority low-income women. So Battaglia has her sights set on a citywide solution, built on diverse community partnerships. She is a founding member of the Boston Breast Cancer Equity Coalition, a group of stakeholders who came together in early 2014 to review available data and discuss strategies to address the problem. The coalition comprises a diverse group with a history of collaboration, including the American Cancer Society, the state and city public health departments, and the many Boston institutions where breast cancer patients receive care. Among the members are oncology and primary care clinicians, patient navigators, public health policymakers, advocates, researchers, and patients. The vision of the coalition is to eliminate the differences in breast cancer care and outcomes by promoting equity and excellence in care among all women of different racial or ethnic groups in Boston. And Battaglia is leading efforts to secure research funding so the coalition can identify citywide solutions.
This Series
Also in
Breast Cancer Research
-
April 24, 2017
Zebrafish Cancer Genetics Illuminate Human Breast Cancers
-
April 24, 2017
Dioxins Point to Targets for Treating Breast Cancer
-
April 24, 2017
Too Many Black Women Die from Breast Cancer. Why?








Comments & Discussion
Boston University moderates comments to facilitate an informed, substantive, civil conversation. Abusive, profane, self-promotional, misleading, incoherent or off-topic comments will be rejected. Moderators are staffed during regular business hours (EST) and can only accept comments written in English. Statistics or facts must include a citation or a link to the citation.