Medical Campus Experts Gather to Confer about Zika
NEIDL acquires sample of virus for further study
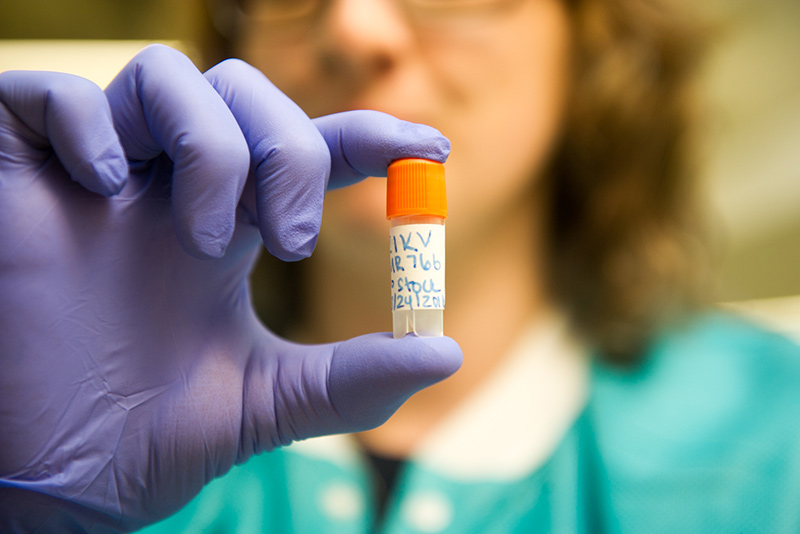
BU’s NEIDL received a sample of Zika earlier this week, which will allow scientists to grow and propagate the virus for study.
After weeks of Boston University researchers trying to procure a sample of Zika virus, the pathogen linked to microcephaly and other neurological syndromes, the vial finally arrived at BU’s National Emerging Infectious Diseases Laboratories (NEIDL) on March 22, 2016. NEIDL director Ronald B. Corley, a BU School of Medicine (MED) professor and chair of microbiology, announced the acquisition that day at a Boston University Medical Campus (BUMC) Provost Research Seminar. Zika, like dengue, mumps, and measles, is a Biosafety Level 2 pathogen, defined by the Centers for Disease Control and Prevention (CDC) as an agent that poses “moderate hazards to personnel and the environment.”
The sample was of the strain originally isolated in 1947, and it will allow scientists to grow and propagate the virus for study. The 1947 strain is the precursor to the virus causing the current outbreaks in South America and the Caribbean. Because samples of the modern virus are proving difficult to obtain, scientists at NEIDL will begin their work using the 1947 isolate while using published genetic data to make a clone of the modern Zika strain.
“There’s a real need for us to be doing research on this virus. It’s been seen in Boston and will be again,” said John Connor, a MED associate professor of microbiology and a NEIDL researcher, who acquired the Zika sample from the Biodefense and Emerging Infections Research Resources Repository, a supply house for scientists studying infectious diseases. “Having the virus will allow us to ask important questions, like: what is driving the pathogenesis? How is the virus getting across the placental barrier? What is its replication like in mosquitos?” Connor said. “Without understanding the virus, it’s hard to know how to block it.”
Karen H. Antman, dean of MED and provost of the Medical Campus, began planning the Zika workshop about six weeks prior, when she became aware that people from BU’s medical, dental, and public health schools were all talking about the virus, but not necessarily collaborating. “It’s a rapidly emerging field—we want everyone doing research on this in the same room,” says Antman. “Clinical people have blood specimens, lab people have techniques. We wanted them all talking to each other.”
Zika grabbed the world’s attention in fall 2015 when scientists in Brazil began to suspect a connection between the virus and microcephaly—babies born with small heads and neurological deficits—and also Zika’s possible link to other neurological syndromes like Guillain-Barré. Since January 1, 2007, 59 countries and territories have reported transmission of Zika virus, according to the World Health Organization (WHO), and on February 1, 2016, the WHO declared the cluster of microcephaly cases and other neurological disorders a health emergency. So far, 258 cases have been reported in the United States, all introduced from other countries.
The Research Seminar, which included updates from virologists, epidemiologists, and physicians, revealed what scientists have learned about the virus since the 2015 outbreak in Brazil and how many questions remain.

“Zika is difficult to diagnose; the clinical symptoms are really vague,” Robin Ingalls, a MED associate professor of medicine and microbiology, said during her clinical overview of Zika. Ingalls noted that an estimated 80 percent of people infected with Zika show no symptoms at all. Most people who get sick have a red, pimply rash that Ingalls called “very subtle,” along with other symptoms—like fever, headache, fatigue, and malaise—that overlap with dengue fever and chikungunya, making the disease even more difficult to diagnose.
Lab tests “don’t really make it much easier,” she said. “While we can detect virus in the blood, it is only there for about a week after infection.” After the first week, physicians can order blood tests that measure antibodies specific to Zika. Laboratories are reporting a backlog in these tests, however, with results taking as long as six weeks. Also, the tests can be difficult to interpret because of cross-reactions with similar viruses, like dengue, the patient may have been exposed to.
Many questions about transmission, especially from mother to fetus, remain unanswered, Ingalls said. “How can Zika evade the immune response of placenta? What is the critical time for exposure of the fetus? Is there something unique about Brazil that is increasing the risk of microcephaly?” she asked. “We’re just seeing the tip of the iceberg, and we don’t know what the long-term consequences of infection will be.”
“It appears pretty convincing that Zika is linked to microcephaly,” said Donald M. Thea, a BU School of Public Health (SPH) professor of global health and director of the BU Center for Global Health & Development, who spoke on the public health aspects of Zika. “From an epidemiological perspective, the question is, how high is the risk?”
Much of Thea’s talk focused on what scientists know about the transmission of Zika from mosquitos to humans, and from one human to another. He noted that scientists have isolated the virus from 10 species of Aedes mosquito, and from several other mosquito families as well. While Aedes aegypti is the best known, he said, Aedes albopictus—introduced into the United States in 1985—is the most worrisome because of its hardiness and wider range. “If efficient transmission is limited to Aedes aegypti, then the virus shouldn’t get beyond Texas and the southeastern United States,” areas with warm, moist air where that mosquito can thrive, he said. But if Aedes albopictus can spread the disease just as well, larger areas of the world may be exposed.
Thea also explained what scientists currently know about human-to-human transmission. They have found that patients carry low levels of Zika virus in their blood after symptoms begin, but higher levels of the virus in urine, saliva, and semen for a longer time. (Scientists have also found Zika virus in cerebral spinal fluid and in breast milk.) Thea said that the risk of transmission through semen is especially worrisome. “The amount of virus in semen is very high,” he said, noting that the viral count in semen can be 100,000 times higher than that in blood, and that scientists have measured Zika virus in semen as late as 62 days after infection. “A patient’s semen contains virus before the onset of symptoms, but we’re not sure how long the virus remains infectious. We are at the cusp of a really interesting part of the Zika virus investigation.”
Also speaking at the seminar were Davidson Hamer, Athanasios I. Zavras, and Rachel Fearns. Hamer, an SPH professor of global health, explained how the GeoSentinel Network—a clinic-based global surveillance system that focuses on travelers, immigrants, and refugees—allows scientists to detect new infections and disease patterns, all with lab-confirmed diagnoses. He expects to publish preliminary GeoSentinel Network findings on Zika in the coming months. Zavras, a BU School of Dental Medicine professor and chair of pediatric dentistry, discussed the detection—and possible transmission—of Zika virus through saliva. Fearns, a MED associate professor of microbiology, described mutations in the Zika genome that may be helping the virus replicate, and spread among people, more efficiently.
“Up until about four years ago, proposing to study Zika was a dead end for funding. It wasn’t very prevalent,” Connor said during a discussion panel at the end of the seminar. “It’s only the recent rapid spread and new adverse outcomes associated with infection that have made research to understand this virus a high priority.”


Comments & Discussion
Boston University moderates comments to facilitate an informed, substantive, civil conversation. Abusive, profane, self-promotional, misleading, incoherent or off-topic comments will be rejected. Moderators are staffed during regular business hours (EST) and can only accept comments written in English. Statistics or facts must include a citation or a link to the citation.