Insights into Neurovascular Coupling Hold Promise for Post-Stroke Monitoring and Recovery
Results from a new study examining the relationship between neural activity and cerebral blood flow after a stroke will help make neuroimaging techniques like fMRI more reliable for monitoring and guiding recovery.
By Jim Cooney
According to the CDC, more than 795,000 people have a stroke in the U.S. every year, and while the majority do survive, stroke remains the leading cause of serious long-term disability.
Post-stroke recovery typically involves highly individualized rehabilitation treatments which, in turn, rely upon various forms of feedback to guide the treatments and monitor success. Neuroimaging techniques, such as functional magnetic resonance imaging (fMRI) and functional near-infrared spectroscopy (fNIRS), hold tremendous potential for providing such feedback. By allowing clinicians to observe blood flow activity within the brain, neuroimaging provides insights into the associated activity of neurons—a tight relationship between neural activity and cerebral blood flow known as neurovascular coupling, or NVC.
However, while NVC tends to be a stable and reliable association in healthy subjects, past studies have demonstrated that brain pathologies like stroke, Alzheimer’s disease, and traumatic brain injury can significantly disrupt NVC. While this “uncoupling” is not yet well understood, it would potentially make neuroimaging an unreliable source of information for clinicians treating stroke victims.
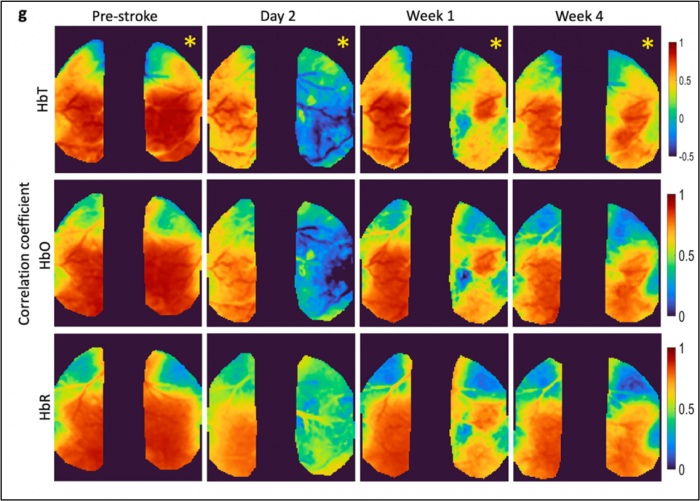
Thankfully, a new NIH-funded study published in Neuroimaging, which simultaneously measured cerebral blood flow and neural activity in rodents before and after a stroke, demonstrated that after an initial uncoupling effect observable in the hours and days following a stroke, NVC resembling pre-stroke activity was again observable in as little as two weeks.
Dr. Smrithi Sunil, lead author of the study, says these findings have effectively unlocked the potential of neuroimaging as reliable tools for guiding rehabilitation after a stroke. “Using techniques like fMRI and fNIRS, we can provide more individualistic rehabilitative therapies, monitor the progress of these patients, and then change the therapies accordingly, because we know how to better interpret what the neuroimaging data is telling us.” Prior to assuming her current role at the Allen Institute for Neural Dynamics, Dr. Sunil had been working in the Boston University Neurophotonics Center as a PhD candidate.
Previous research on functional recovery after stroke, even when using animal models, has tended to focus primarily on either neural activity or cerebral blood flow, with very little work attempting to integrate the two. This study utilized a wide-field multimodal imaging technique that allowed researchers to simultaneously and longitudinally monitor both kinds of activity during stroke recovery, thus giving them a detailed picture of the evolution of NVC across the surface of the brain. In commenting on the unique neuroimaging techniques involved, Professor Anna Devor (BME), a coauthor who runs the Neurovascular Imaging Laboratory at BU which collaborated on the study, says, “This line of research provides a perfect application arena for our neurophotonic tools, in particular those for imaging of blood flow and oxygen metabolism in mouse models of human disease.”
Professor David Boas (BME, ECE), director of the Neurophotonics Center and head of the Bio Optical and Acoustic Spectroscopy Lab—where the research was primarily conducted—said the study produced additional findings that have since led to a new NIH grant. “The unexpected observation that increased vascular oscillations one week after stroke predicted better behavioral outcomes at week four has motivated us to more closely examine the coordination of excitatory and inhibitory neural activity in driving functional repair post-stroke.”
Dr. Sunil says the study’s implications may extend beyond improved guidance and monitoring of stroke recovery too, allowing clinical researchers to, for instance, use neuroimaging to discover more about the mechanisms underlying stroke recovery, which may in turn lead to the development of new therapies. Improved study of stroke recovery, Sunil says, also has parallels to other neurodegenerative disorders like traumatic brain injury or Alzheimer’s, “So while we’ve studied mainly stroke so far, we could use the whole imaging pipeline that we’ve set up to look at neurovascular coupling across other neurodegenerative diseases as well.”