Racism has been a major societal issue since the beginning of time, and unfortunately, it’s not a thing of the past. Today especially, it’s speaking just as loud as it was decades ago. But now with COVID-19 in the mix of the current social justice movements, it’s important to talk about how the two intertwine with each other and how racism is very relevant to the healthcare system. In the newest Smarter Healthcare podcast, episode 8, Sandro Galea, MD, MPH, DrPH Dean, of Boston University School of Public Health discusses the social determinants of health, as well as COVID-19 and racism in healthcare.
“The Great American Trauma”
2020 has become a year to remember. Time and time again, unrecoverable events have been bubbling up to the surface of our country and our world, and they all seem to be connected in some way. Sandro Galea calls this “The Great American Trauma,” and discusses the concepts and connection to social determinants of health.
“We are going through a period of what I’ve called ‘The Great American Trauma,’” says Galea. “One of them is obviously COVID, the pandemic itself, the other one is unemployment and the economic consequences, and the third one is a reckoning with decades-old, centuries old, racial injustice, deep-seated structural racism. By social determinants of health, we mean the forces that drive health that are outside of our bodies. So, it’s not the biological determinants. Social determinants are the housing we live in, the transportation we take to work, the air we breathe, the water we drink, whether there’s gender equity, whether we are victims of violence, whether there are opportunities to actually live one’s life fully. And when we think about health, historically we have taken a very biomedical approach to health. Which means we have privileged the biological determinants.”
In relation to COVID-19, Galea says that it’s important to recognize that the social determinants are what shapes our health.
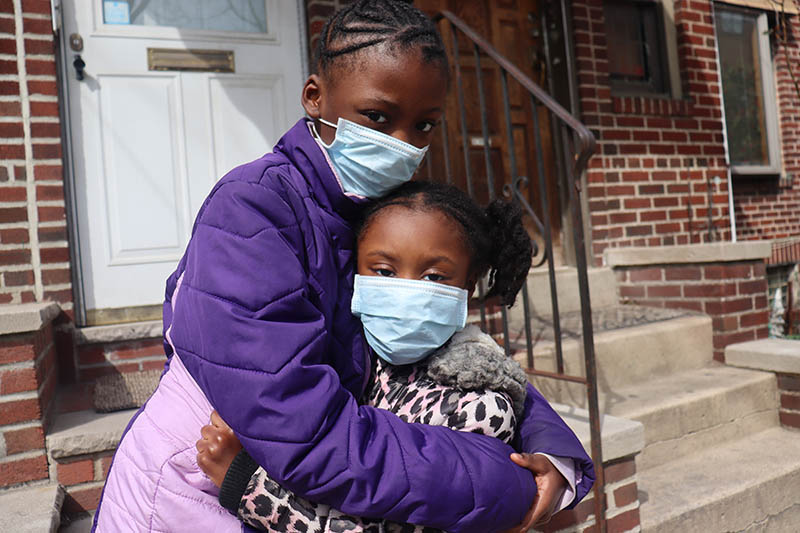
Mortality and healthcare access
In New York City’s case, some predominantly Black neighborhoods in the Bronx and Brooklyn had a death rate twice as high as those in white neighborhoods. Galea recommends thinking about this statistic as two sets of risks: contracting COVID and getting really sick with COVID. The risk of contracting the virus is determined by a number of factors such as social distancing abilities, which is in fact a privilege that many don’t necessarily realize. Black workers are in fact more likely to work in service industries and occupations that lower their ability to social distance, which not only puts themselves at risk, but their families and their communities as well. Even with proper equipment (i.e. masks, plexiglass shields, etc.), occupational steering also means fewer financial resources if a Black individual were to get COVID due to low wages, decreasing Black individuals’ options for good health insurance, emergency savings, and living expenses. All of these factors lead to a higher chance of African-Americans not only going into medical debt if they get the virus, but also a lower chance of survival and care, which is not the case for white individuals.
Another factor of health disparity in relation to COVID-19 is the fact that African-Americans are more regularly exposed to health hazards than whites. According to Forbes, “several books have documented that Black families often live in communities with worse air and water quality than white families,” and that Black children are also more likely to suffer from asthma due to persistent housing segregation. And since COVID-19 is a respiratory virus, it’s clear that a sufferer of asthma or bad air quality would be more likely to contract stronger and possibly even fatal side effects if they caught the virus.
Black families also have a higher chance of living in food deserts, which is where the access to healthy food options is little to none. Both grocery stores and restaurants are included in the food desert issue as healthier options usually cost more. And as stated previously, African-Americans often have a lower salary than whites, so a lower salary may result in a smaller array of healthy food options for the individual and their family, which often leads to unhealthy outcomes such as obesity and diabetes,- both of which can lower the immune system and give Blacks a higher risk of catching COVID-19.
“If you are born in a poor household and your parents have to work two jobs to keep you fed, and you grow up by yourself, and looking out for yourself, watching TV, you’re going to eat junk food, that’s what your parents can afford, you’re going to grow up obese, that instantly creates greater risk factors for you, it makes it hard for you to lose weight later in life,” Galea explains… “You then move on to a manual labor job where you’re standing on your feet, and by the time you’re in your mid-40s, you have extra weight, you’ve been on your feet all your life, and you need a knee replacement. Now, we can see the knee replacement as a biological factor, saying well, it’s osteoarthritis that resulted in a knee replacement, let’s worry about it biologically. But a social determinant’s perspective says what really drove the knee replacement was your misfortune of being born in poverty, the fact that you got obese in childhood because you had poor eating habits, the fact that you never got a good education, and as a result you ended up working on your feet all your life. So that’s a social determinant’s perspective versus a biological or bio-medical perspective.”
Protests
In the podcast, Galea also talks about the protests and the civil unrest that have taken place in the United States and whether they impacted the pandemic response and if they affected outcomes. Galea seems to think that new transmission of COVID was not a direct result of the protests because of the fact that almost all of those protesting were wearing masks and trying their best to social distance, and because of the new knowledge we have of transmission being lower outdoors than indoors. And like many others, he believes that the protests put race front and center, where it should be, regardless of the fact that there’s a pandemic. If anything, the issue of racial injustice has helped to shed even more light on the health disparities among the BIPOC community.
Zinzi Bailey, ScD, assistant scientist at the University of Miami Miller School of Medicine’s Jay Weiss Institute For Health Equity at the Sylvester Comprehensive Cancer Center states that “One could try to argue that police violence alone won’t kill as many people as COVID-19 will… the protesters are protesting more than just the killing of George Floyd. If we don’t fight systemic racism now, that epidemic is going to last generations, and we’ve already had 400 years of doing this.”
Conclusion
When asked about the positive outcomes that may have come out of the pandemic in relation to social determinants of health, Galea again emphasizes the importance of conversation and how social determinants are now being discussed in the context of a pandemic which will hopefully further educate us. He also believes that healthcare leaders should realize that while they may be taking all the right steps to running a hospital, such as restoring health to those that are sick or injured, it’s just as important to understand that people’s health is largely triggered by and shaped by their environment and that as healthcare leaders, they have an important voice that can be part of the solution if they embrace that charge.
Ultimately, 2020 has given us a glimpse into not only the future but the past as well. There are centuries of racism and injustice that are still alive to this day in the midst of a pandemic. These issues will not be solved overnight, but we can all take part in becoming the change. As Jewel Mullen, MD, the associate dean for health equity and an associate professor of public health at the University of Texas stated, “It’s people’s willingness to risk their lives to try to save their lives.”
To listen to the full episode of this podcast and to learn more about Sandro Galea, click here.