In Spanish, it was once called estar roto: to be broken. Today, we call it post-traumatic stress disorder (PTSD), and psychologists have spent decades transforming it from a source of stigma to a treatable condition. But when PTSD is combined with another serious mental illness, like schizophrenia or bipolar disorder, many therapists hesitate to address the PTSD directly. Now, Jennifer Gottlieb, a research assistant professor at BU’s Center for Psychiatric Rehabilitation (CPR), is helping therapists teach patients how to manage both PTSD and serious mental illness at the same time, creating new hope for individuals struck by this debilitating—and all-too-common—combination.
Thanks to a Senior Researcher Fulbright Award, Gottlieb is preparing to bring this new approach to Spain. Under the two-year Fulbright grant, she will spend a total of six months in Spain, collaborating with colleagues at Complutense University and the Fundación Manantiales mental health center in Madrid. She will begin by training a small group of mental health practitioners in a castellano Spanish–adapted version of the therapy program that she has been developing in the United States. She’ll also be scrutinizing the results of the therapy to see how effective the adapted therapy is in this new cultural context.
“PTSD is a set of symptoms that comes up following a traumatic event, from natural disasters to unexpected death of a loved one to severe childhood abuse,” says Gottlieb. Assailed by flashbacks and anxiety, sufferers may go to extremes to avoid any situation that reminds them of their trauma. “Their life becomes very constrained,” says Gottlieb. Not surprisingly, depression, sleep disturbances, and substance abuse often go together with PTSD.
The good news: There are many PTSD treatments that have been proven to work in the general population. But people with serious mental illness are usually excluded from PTSD treatment studies, despite the fact that they are as much as 10 times more likely to experience a traumatic event and are more vulnerable to PTSD after that trauma. In fact, psychologists estimate that some 25 to 40 percent of people with serious mental illness also have PTSD. “If you have PTSD and a serious mental illness, everything is worse for you,” says Gottlieb, who points to more suicidal thoughts, more ER visits, and symptoms that are more severe and more disruptive to everyday life. “It’s a huge problem, and unfortunately it’s gone largely unrecognized and largely untreated.”
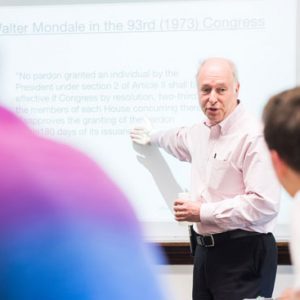
Over the last 10 years, though, researchers have started designing and testing PTSD treatments to meet the unique needs of people who have serious mental illness. The 16-week therapy that Gottlieb will bring to Spain was first developed by Kim Mueser, the CPR’s executive director, and uses an approach called “cognitive restructuring,” a type of cognitive behavioral therapy, to help therapy clients recognize and change the paralyzing beliefs that have built up around their trauma, such as distrust and self-blame.
“No matter your trauma or your background, people have these universal beliefs,” says Gottlieb, “whether you’re an older man who’s a combat veteran or a 16-year-old who was sexually assaulted.” The program has already been tested with some 350 patients in New England and New Jersey, with striking results: PTSD symptoms were less severe, distress and depression were reduced, and the poisonous litany of trauma-related beliefs was quieted.
Cognitive behavioral therapy still isn’t widely available for people with serious mental illness in the United States, but the gap is even bigger in Spain, Gottlieb learned on a visit to Complutense University in Madrid in 2014. “Clinicians really want this training, but it’s just currently not a part of what’s going on at these mental health clinics,” she says. Searching for a way to continue her collaboration with her colleagues in Spain, Gottlieb decided to pursue the Fulbright award, which is dedicated to international educational and scholarly exchange.
Gottlieb will take her first Fulbright trip this winter, when she will recruit and train 5 to 10 therapists as they begin applying the treatment with their clients. At the same time, she will be collecting and analyzing data about clients’ progress. In 2016, she will return to expand the program and improve it, based on what she and her colleagues have learned. She hopes that, ultimately, the clinic will screen every patient for PTSD so that they can get appropriate treatment.
“To be granted the Fulbright is a tremendous honor,” she says. “And it is a dream come true to combine this work that I love and feel is so important with a culture and a country that I feel really tied to as well.”





































Related Stories
Patient-Centered Team Treatment of Schizophrenia Works Best
SAR prof senior author on landmark study
Two Professors Win Fulbright Awards
Samuel Hammer will go to Sri Lanka; Meg Tyler to Belfast
BU Spearheads Largest-Ever Study of Child Anxiety
Will compare online versus in-person therapy
Post Your Comment