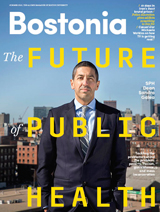
When the bombs went off at the Boston Marathon finish line last April, Jonathan Woodson found himself fielding emails in his Pentagon office from former colleagues in Boston seeking advice on how to care for trauma victims who had lost limbs.
After three years as the top health official for the US Department of Defense, Woodson had seen the synergy between battlefield and civilian medicine from both sides. As a School of Medicine professor of surgery and a vascular surgeon at Boston Medical Center, he had looked to advances in military medicine to inform his own civilian practice.
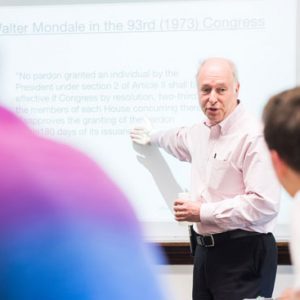
“There’s a yin and yang” between military and civilian medicine, Woodson said on Monday, when he delivered the 10th annual Pike Lecture on Health Law, hosted by the School of Law and the School of Public Health. “Many of the strategies we have developed to save limbs in wartime have been transferred to civilian practice,” he told his audience.
As the war in Afghanistan winds down after more than a dozen years, the challenge for medical professionals is to secure the partnerships that will allow for close collaboration between the military and civilian medical systems, he said, to ensure that advances in treatment and technology are shared.
Nominated by President Obama as assistant secretary of defense for health affairs in 2010, Woodson noted that the last 13 years of war have been “unprecedented” for the United States—not only in terms of length, but in the challenges posed. The use of improvised explosive devices, or IEDs, has intensified the severity of injuries, prompting medical advances in trauma treatment, limb salvage, and prosthetics.
Woodson’s lecture, titled Meeting the Needs of America’s Heroes: A Lifetime and Community Obligation, offered insight into the responsibilities the nation has to military ill or injured as a result of their service in Afghanistan and Iraq. He said that military medicine has adapted well despite a rise in the severity of injuries, with the combat death rate falling from 2005 to 2013, but that “greater salvage of life” has posed new challenges, as the medical system now must find ways to meet the holistic needs of the wounded over the long term—a task that includes treating “the mind, body and spirit. The whole idea is that we have a responsibility for making the wounded warrior whole…and more importantly, we have to make that commitment for decades.”
While there have been significant technological advances in treating amputees, many of the service members wounded suffer from so-called invisible wounds: traumatic brain injury (TBI) and post-traumatic stress disorder (PTSD). More than 280,000 troops have suffered traumatic brain injuries since 2002.
Woodson acknowledged that while there have been advances in treating those injuries, “we’re really at the nascent period of understanding neuroscience…We don’t yet know much about the long-term outcome” of TBI or PTSD.
He said many of those injured veterans will need care for years to come—a challenge that will require a public-private partnership of government, community, academic, and philanthropic organizations. “We have met some of the challenges, but there is clearly more to do.”
Woodson, a brigadier general in the US Army Reserve, noted that the recent wars are the first time that service members have been deployed to combat multiple times—some of them for fifth and sixth tours of duty. The effects of those repeat deployments are still unclear, he said, explaining that there has been no clear correlation found between multiple deployments and the incidence of PTSD.
“We haven’t quite sorted out the story about repetitive deployments and PTSD,” he said. There is evidence that some troops who deploy multiple times may have some “protective mechanism” or resilience that guards against psychological injury. “The bottom line is, we’re not sure what multiple deployments mean,” in terms of psychological impacts.
Because the United States has an all-volunteer force, many troops want to continue on active duty, even after suffering major injuries, Woodson said. That desire to retain a “military identity” has prompted the armed services to find ways to accommodate injured service members on active duty, sometimes in command or support positions. About 20 percent of amputees return to active duty, for example.
“In a professional force, one of the issues is, people want to go back….They define themselves as soldiers, sailors,” he said. “It’s a complicated situation that I don’t know if we fully understand at this time.”
Woodson’s visit to BU came as School of Public Health researchers are immersed in several projects related to veterans’ health, including piloting a web-based intervention that focuses on self-management to reduce unhealthy drinking in veterans with PTSD. Another ongoing project is a large-scale study of veterans of the Gulf War that is examining whether chronic inflammation in the brain, caused by chemical exposure, is a trigger for multisymptom illness.
Woodson, who also was MED associate dean for diversity and multicultural affairs before taking the post as assistant defense secretary, said that collaborations with academic institutions are key to ensuring that wartime lessons are incorporated into civilian medicine, and that best practices are shared.
“We’ve got a whole generation of injured individuals who started out at age 20” and will need care into their 60s and beyond, he said.
The annual Pike Lecture on Health Law honors N. Neal Pike (LAW’37), a distinguished lawyer and lifelong advocate for individuals with disabilities.





































Related Stories
School of Medicine Launches Military Health Center
Coordinating the University’s military-focused research and service projects
Former DOD Official Heads New BU Health Innovation Institute
Jonathan Woodson, brigadier general, was MED associate dean
Easing Transition to Civilian Life for Women Veterans
MED researchers create network with Walmart Foundation grant
Post Your Comment