Three years after President George W. Bush limited federal funding for human embryonic stem cell research, a solid majority of California voters cast ballots in favor of Proposition 71, also known as the California Stem Cell Research and Cures Act, which asserts a state’s constitutional right to carry out stem cell research. The 2004 law led to the creation of the California Institute for Regenerative Medicine (CIRM), which funds stem cell research that seeks therapies or cures for conditions like Alzheimer’s disease, ALS (amyotrophic lateral sclerosis), cancer, and Parkinson’s disease.
Coincidentally, that same year California voters narrowly defeated a proposition that would have required sizable companies to provide health insurance to their employees. The election results seemed to indicate that voters were more concerned about pushing the boundaries of science than providing neighbors with access to basic health care.
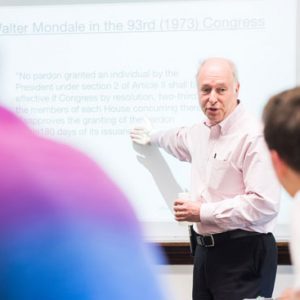
Ruha Benjamin, a College of Arts & Sciences assistant professor of sociology and African American studies, witnessed these debates as the sole social scientist CIRM invited to study the ethical, legal, and social implications of stem cell research while she was a doctoral student at the University of California, Berkeley. Benjamin explores the controversy surrounding California’s stem cell research initiative and the bioethical questions it’s raised in her new book, People’s Science: Bodies and Rights on the Stem Cell Frontier (Stanford University Press, 2013), which draws on her observations at CIRM. She addresses the social impact of stem cell research and how the voices of women, minorities, and members of the disabled community were ignored during CIRM’s founding.
Bostonia spoke with the author recently about her observations at CIRM, whether women should be paid for the eggs they donate to research facilities or infertility clinics (from which stem cell researchers often draw tissue), and the need to reimagine the way children are taught science.
Bostonia: How did you come across this research opportunity?
Benjamin: Part of the funding for the stem cell agency allotted money to train new scientists to come up in the ranks. They decided they would have one law student and one social science student be part of an otherwise all-bioengineering cohort. I was the one social scientist brought into the fold. What that usually means is that you study the effects of what the scientists are going to do, but don’t turn your lens on the scientists themselves. They’re doing their work, so don’t turn the analytic gaze back at them and say, “What are your values? What are your norms? What are your interests?”
So they thought you would write about the positive impacts of stem cell research?
What was constantly being asked of me was whether I could figure out why some people are not on board, why these communities don’t trust us, why don’t they sign up to be part of our clinical trials. That’s the role of the social scientist: to study those who are refusers and to help us reach them. Give us what you find so that we can bring them on board. Never mind figuring out why so many people are exuberant about something that is all promise. That’s where I try to be more ecumenical. That’s fine. Let’s study distrust, but at the same time let’s figure out why people trust and believe in this so much.
Did CIRM officials give much thought to which groups should be included in discussing the potential benefits or pitfalls of stem cell research?
They have an Independent Citizens Oversight Committee, and—from their perspective—it’s very inclusive. They have dedicated 10 seats on this board for different diseases. They’re not everyday folks who are stomping the pavement trying to get funding. They’re directors of huge multimillion-dollar centers who represent these diseases. For anyone to become a member of this board, they go through vetting, but the vetting has included a kind of litmus test to see if you’re a true believer. If you don’t pass, and if you sound at all like you might slow this process by bringing in a disability perspective or a strong feminist critique of payment for eggs, then they find someone else.
According to your book, everyday stem cell advocates are most often parents or caregivers, but not the people living with a particular condition or illness. Why do you think that is?
That’s definitely a characterization for most patient advocacy groups. Partly it’s because, healthwise, they can do it. Perhaps people that they’re advocating for have to deal with a lot of day-to-day things that keep them from lobbying and making calls.
Another perspective is that, especially for people who are born with a condition that they’re used to, they’re part of a community of other similar people. Their interest is to be able to live their life fully, to be respected, and to see themselves as contributing to their community. So you have to choose. How are you going to spend your time? And for many people, it’s about living life to the fullest and not spending hours on end every day advocating for cures—especially knowing that the majority of these treatments are not going to be seen in their lifetime, if ever.
I was surprised to read about the complications women endure from the egg extraction necessary to donate eggs for research or for infertility treatments.
Most of the stories of people being harmed through multiple egg extraction never reach the light of day. Unlike people who are using egg donors to create babies, in research you don’t need to worry about a woman’s level of education or necessarily race. You need the eggs to experiment on. You actually might want a more diverse range of eggs to have more genetic diversity, which means that more women will be enrolled. Poor women, working-class women, and women of color are more likely to be egg donors for stem cell research than we find in the private sector, because those demographic characteristics are not only disregarded, but researchers actually want that diversity.
What’s your opinion about paying donors for eggs?
Until we have prioritized the health of women and tracked long-term what the effects of multiple egg extraction are, then we shouldn’t be paying. Do we want to incentivize women putting themselves in harm’s way if we haven’t even tracked what the health effects are? We hear about how many babies are born every year through this process, but we’re not told how many women die of complications or suffer from ovarian hyperstimulation syndrome. We’re tracking the positive, but not the negative.
Many stem cell advocates worry that including the perspectives of diverse groups of people might slow down the pace of scientific discovery. Do they have a point?
Ultimately it’s going to come back to bite us if we don’t include more social representation early on. In an instrumental way, they know this. The federal government requires that researchers have a diverse representation of women and people of color in clinical trials. You might be able to rush the early-stage research, but when you need to translate it into the clinic, you’re going to be slowed down eventually. Now or later, you will have to deal with it.
Where should we start if we want to conduct life science research in an equitable manner?
Where I would put my energy and effort is in a long-term rethinking of how we make everyday people a part of science. The way most students are taught science is that you learn the facts, you learn the experiments, but you don’t learn to think critically. I talk about one initiative in a magnet school in the Watts area of Los Angeles, where they’re teaching kids not just about genetic technologies and stem cell research, but having them ask questions about what this means for them, what does this mean for their community, what are the possible negative implications of some of this, and what are the promises.
In the short term, the way we think about who should be at the table shouldn’t be as instrumental as it has been. We need to think about who can raise the issues in a way that has to do with disability rights and women’s health. These have to be seen as part and parcel of making good science and not simply something that’s there to stump the researchers.





































Related Stories
CReM Stem Cell Researcher Is Innovator of the Year
MED’s Gustavo Mostoslavsky invented tool facilitating cell production
CReM Honored for Sharing Stem Cell Lines
Team wins award from Association of American Medical Colleges
POV: Unregulated Stem Cell Clinics Pose Real Threat
Problem growing in US
Post Your Comment