Battling Ebola: How Ebola Kills
MED’s John Connor is devising diagnostics to spot Ebola and antivirals to treat the disease
On Saturday, the first of two sickened American health care workers was flown from Africa to a special containment unit at Emory University. Despite the risk of infection, medical personnel continue to travel to West Africa to help bring under control the worst Ebola outbreak on record, which has killed more than 900 people to date. The World Health Organization plans to spend $100 million to fight the outbreak, and the Centers for Disease Control and Prevention will send 50 more aid workers. In this weeklong Special Report, BU Today talks to Boston University researchers in several fields about why medical personnel confront the risks; the ethical and political dilemmas presented by the outbreak; how the virus kills; efforts to design effective therapies; and other aspects of this unprecedented outbreak of Ebola.
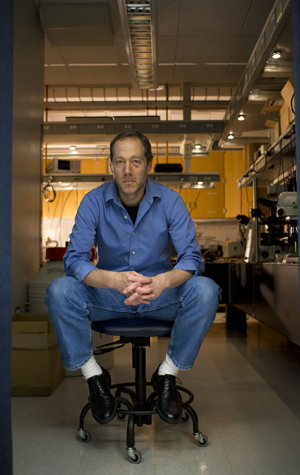
The Ebola outbreak in Guinea, Sierra Leone, and Liberia has now infected more than 1,600 people, according to the World Health Organization. To learn about how the virus kills and efforts being made at BU to devise diagnostics and therapies to treat it, BU Today spoke with John Connor, associate professor of microbiology at the School of Medicine and a researcher at Boston University’s National Emerging Infectious Diseases Laboratories (NEIDL). Connor, whose research is funded by the National Institute of Allergy and Infectious Diseases, studies the tricks that viruses use to dominate their cellular hosts. He has been working collaboratively with researchers at BU and at other research institutions, with a particular focus on the Ebola virus.
BU Today: What aspect of the Ebola virus is the focus of your work?
Connor: My lab is interested in several different approaches to try to understand and stop diseases caused by viruses like Ebola. This includes the development of antivirals, vaccines, and point-of-care diagnostics, in collaboration with the Photonics Center and the lab of Selim Unlu, College of Engineering associate dean for research and graduate programs in the department of computer and electrical engineering.
Another thing we are looking at is what goes wrong with the immune response during viral infection. Our bodies are so good at responding to so many diseases, and in most cases we get sick for a couple of days and then we get better. Our response to Ebola is totally out of whack. The immune system appears to deliver a much more aggressive response than is necessary, one that causes a lot of damage to the body. That overreaction is a significant part of what makes infection with this virus so deadly.
What kind of damage is done by the overreaction?
The response is so strong that it triggers other pathologies. This can include diffuse intravascular coagulopathy, which is why the virus is often called a hemorrhagic fever virus. Normally, coagulation is constantly serving your body, so if you get cut you get a nice blood clot that seals you up. It’s a great way to keep your blood from leaking out. In the case of Ebola, you get clotting in inappropriate places, such as organs like the liver. The problem is, you have a finite number of clotting factors in your body, and they get depleted from the inappropriate clotting. When that happens, you have a hole in your body that needs clotting but won’t stop bleeding. All the small things that happen on a daily basis that are normally taken care of by coagulation are not working.
Do other viruses cause the same coagulation problems?
Ebola is one of the viruses that are most associated with that type of response. The Marburg virus, a cousin of Ebola, can also cause that response, and Lassa fever viruses can as well. Dengue virus can also cause a hemorrhagic disease, in rare cases.
Does every victim of Ebola hemorrhage?
No, but it happens a lot of the time, whereas in other viral infection such as the common flu, it does not happen.
Why is it that some people infected by Ebola get much sicker than others?
That’s one of the things we are trying to learn, but it’s hard. One of the problems of studying a virus like this is that you don’t have large pools of people to work with. Outbreaks of Ebola are sporadic. If you are studying HIV/AIDS, the prevalence of the disease means that you can readily identify 10,000 people. Ebola outbreaks are not predictable and, thankfully, most previous outbreaks were small. This makes other approaches to understanding the course of disease important to try. We are now collaborating with people at other labs who are using animal models of the disease.
What are you learning about how the virus works?
One of the things we’ve been surprised by is how early the immune system response begins and how robust it is. When we compare this response to other viruses, it appears that the response to Ebola is much stronger than to other types of disease. Also, it appears that specific types of responses are associated with survival from the disease. We are investigating whether this early immune response can be used to develop a diagnostic for early disease. Can we look very early, even before symptoms show up, and identify an immune system response to an Ebola infection?
How is the immune response of survivors different from that of people who die?
We have learned that it’s not just the intensity of the response. It also appears to be the type of responses that develop. One of the things we see in animals that succumb to the disease is one type of immune cell—a type of neutrophil—accumulates, whereas in animals that survive, that immune cell is not as abundant.
Are there any therapies that are effective?
There are no Food and Drug Administration–approved therapies. People are beginning to develop some therapies, and information from those studies says that the earlier an individual is treated, the better their survival.
If we can find ways to diagnose infection early, that will directly help effective therapy. And with early diagnosis, if you identify one patient that is symptomatic, suggesting that their course of disease is far along, early tests like the one we are developing will allow rapid testing of contacts of that first patient and early treatment of those infected with the disease.
We are really trying to understand what this very overactive immune response is and how we can start damping it down. Our lab is also developing antivirals that work against Ebola, and we are working on diagnostics that will be at the point of care. We have been focusing on developing a diagnostic for Ebola, Marburg, and Lassa, where point of care is a high priority. We are doing this with the Unlu laboratory at BU, with collaboration from BD Technologies and a spin-out company, NeXGen Arrays, which was started by BU alums and is primarily interested in developing these assays. We are also developing second-generation vaccine viruses in collaboration with Tom Geisbert, former associate director of the NEIDL. The collaboration started when Tom was at BU and has continued since his move to the University of Texas Medical Branch.
Tomorrow: Tracking the Ebola virus. Read all stories in our series “Battling Ebola” here.
Comments & Discussion
Boston University moderates comments to facilitate an informed, substantive, civil conversation. Abusive, profane, self-promotional, misleading, incoherent or off-topic comments will be rejected. Moderators are staffed during regular business hours (EST) and can only accept comments written in English. Statistics or facts must include a citation or a link to the citation.