To read the full story click here.
News
Congratulations to Katherine Gergen Barnett and co-authors for the publication of their article”Warm Handoffs and Attendance at Initial Integrated Bahvioral Health Appointments” in the peer review research journal Annals of Family Medicine.
Click here to read the full story.
Congratulations to Brian Penti and co-authors for the publication of their manuscript “The Role of the Physician When a Patient Disclosures Intimate Partner Violence Perpetration: A Literature Review” in the Journal of the American board of Family Medicine.
Click here to read the full article and press release.
 Congratulations to Suzanne Mitchell who is first author of this important paper from the national PCORI funded Project Achieve research group!
Congratulations to Suzanne Mitchell who is first author of this important paper from the national PCORI funded Project Achieve research group!
Click below to see Dr. Mitchell’s paper and press release!
Mitchell ACHIEVE Focus group paper
Dear DFM faculty, residents and staff,
It is my pleasure to announce that Jeff Markuns MD, EdM has recently been hired in a new role as the Deputy Director of the Primary Health Care Performance Initiative. Jeff will carry out this new role from the BU-DFM and remain on the faculty. The PHCPI is a Gates Foundation-funded program bringing together the World Health Organization, the World Bank, Ariadne Labs and Research for Development in a consortium committed to developing new indicators and ways of measuring primary health care in low and middle income countries, and more generally promoting primary health care as a major agenda item for all institutions involved in global health. Over the next few months, the PHCPI will be launching a Vital Signs Profile for measuring primary health care systems in low income countries, supporting its use in several exemplar countries, and working alongside the WHO in promoting activities related to the upcoming 40th anniversary of Alma Ata.
Jeff will now be able to bring his considerable experience developed here at BU in global primary care systems strengthening and Family Medicine development to a worldwide stage. Jeff is “thrilled to have this opportunity to work together with such influential partners on a global scale in bringing the new U.N. Sustainable Development Goal for Health to reality: Ensure healthy lives and promote well-being for all at all ages.” Jeff will also continue leading our successful Global Health Collaborative in the DFM as well as BU’s Health Sciences Education Masters and Certificate program here in GMS.
Jeff’s selection for this position is a testament to the remarkable work achieved here in the BU/BMC DFM in global health related to primary care. Please join me in offering congratulations to Jeff on this exciting transition, and I encourage all of you to follow the work of the PHCPI in the coming months (www.phcperformanceinitiative.org).
Sincerely,
Congratulations to Paula Gardiner and her co-authors in the DFM — Katherine Gergen Barnett, Brian Penti, Rob Saper, Pam Adelstein, Ivy Brackup, Christine Farrell-Riley, Lance Laird, and Suzanne Mitchell – for publication of their important article article “Design of the integrative medical group visits randomized control trial for underserved patients with chronic pain and depression” that was published in Contemporary Clinical Trials.
Click the link provided to read the full provider: Published IMGV RCT Methods Paper.
Congratulations to Jeff Markuns, MD, MEd for getting his article “Development and validation of the Vietnamese primary care assessment tool”published!
 Congratulations to Jeff Markuns, MD, MEd for publication of the important article “Development and validation of the Vietnamese primary care assessment tool” in which he and his colleagues adapted the PCAT Primary Care Assessment Tool for Vietnam. This work will allow formal assessment of the rapidly growing family medicine sector within Vietnam that Jeff and his team have been so involved with for many years.
Congratulations to Jeff Markuns, MD, MEd for publication of the important article “Development and validation of the Vietnamese primary care assessment tool” in which he and his colleagues adapted the PCAT Primary Care Assessment Tool for Vietnam. This work will allow formal assessment of the rapidly growing family medicine sector within Vietnam that Jeff and his team have been so involved with for many years.
Click here to read the full article!
The Hero of Preconception Care
BOSTON – Health care might have found its Wonder Woman. She can identify health risks in young African-American women and help them successfully resolve those risks. She is engaging, empathetic, culturally competent, and extremely knowledgeable in preconception care. And soon, her advice will be available at any time to participants in a new study at Boston Medical Center meant to overcome factors that are detrimental to black women’s health, like limited physician time and resources.
She can also be everywhere at once because Gabby, a significant healthcare disruptor, is not a real, physical person. The Gabby Preconception Care system, her formal name, is an embodied, online animated character, delivered via computer or tablet screen. She is programmed and designed to screen young black and African-American women for more than 100 general and reproductive health risks and to help them resolve those risks for before pregnancy.
“Gabby is part of a new effort to focus on engaging young women before they become pregnant – a concept called preconception care,” said Brian Jack, MD, chief of family medicine at Boston Medical Center. “Essentially, healthy women are more likely to have healthy babies.”
Despite decades of research, health disparities in birth outcomes persist for black and African-American women, who are more than two times as likely to deliver a low-birth weight infant as white women. Intervention studies in prenatal care have not been shown to lessen persistent disparities in birth outcomes, and it may be too little, too late in attempts to resolve concerning health disparities. In addition, there has been only modest progress in implementing what is known about preconception care into clinical practice, and little research has been done to translate preconception care knowledge into health delivery systems.
Jack’s team has spent the last six years developing, refining, and studying Gabby to fill that delivery gap in preconception care. She represents a prototype for the future of health care delivery by aligning with current technology and supplementing the care provided by community-based health providers.
Gabby faces her next test in real-world clinical settings at six Healthy Start and six Community Health Center sites. The new study, which is supported by a $1.58 million grant from the Agency for Healthcare Research and Quality (AHRQ), will recruit 60 black or African-American women to interact with Gabby over six to nine months – at times decided by users.
Gabby has been successful in her mission to reduce pregnancy health risks before. In a randomized control trial, Gabby identified and successfully resolved health risks by more than 25 percent compared to a control group. Almost two-thirds of participants in the trial reported they used information from Gabby to improve their health, and another 22 percent planned to do so in the future.
“Gabby’s ability to deliver content in a simple, conversational style is the closest person to person communication a device can provide. Her nonverbal conversational behaviors also enhance recall of critical information, as education is the key to the Gabby System and mitigating health risks,” said Jack, who is also a professor and chair of the department of family medicine at Boston University School of Medicine.
The content of the Gabby system is tailored to women’s desired outcome and is based on the Centers for Disease Control and Prevention “Content of Preconception Care.” For example, Gabby can tell the difference between women who are interested in pregnancy prevention versus women who want to become pregnant. Gabby delivers specific health behavior change dialogue using techniques like motivational interviewing and shared decision making.
Subjects in the study will be able to create a “My Health to-Do List” during and after their interactions with Gabby, which they can share with their medical providers. Post study, Jack plans to release an implementation toolkit to facilitate broader dissemination of Gabby.
“The Gabby System is designed to extend the patient-provider conversation beyond the office,” Jack said. “Gabby won’t replace the interaction between patients and providers, but instead serves as a catalyst for discussions between them. She’s another resource that can be offered by providers to ultimately facilitate the invaluable, and often time-consuming work clinicians intend to accomplish with their patients, but do not always manage to do so.”
More information on the Gabby System and study grant can be found on AHRQ’s website.
About Boston Medical Center
Boston Medical Center is a private, not-for-profit, 487-bed, academic medical center that is the primary teaching affiliate of Boston University School of Medicine. It is the largest and busiest provider of trauma and emergency services in New England. Committed to providing high-quality health care to all, the hospital offers a full spectrum of pediatric and adult care services including primary and family medicine and advanced specialty care with an emphasis on community-based care. Boston Medical Center offers specialized care for complex health problems and is a leading research institution, receiving more than $117 million in sponsored research funding in fiscal year 2016. It is the 13th largest recipient of funding in the U.S. from the National Institutes of Health among independent hospitals. In 1997, BMC founded Boston Medical Center Health Plan, Inc., now one of the top ranked Medicaid MCOs in the country, as a non-profit managed care organization. It does business in Massachusetts as BMC HealthNet Plan and as Well Sense Health Plan in New Hampshire, serving 290,000 people, collectively. Boston Medical Center and Boston University School of Medicine are partners in the Boston HealthNet – 14 community health centers focused on providing exceptional health care to residents of Boston. For more information, please visit http://www.bmc.org.
Boston Student Selected for Family Medicine Leads Emerging Leader Institute Jin is one of 30 Participants
 Boston, MA- Helen Jin is one of just 30 scholarship winners nationwide selected to participate in he Family Medicine Leads Emerging Leader Institute. Jin is a 4th year medical student at Boston University. As a scholarship winner, Md. Jin will participate in a year-long leadership development program.
Boston, MA- Helen Jin is one of just 30 scholarship winners nationwide selected to participate in he Family Medicine Leads Emerging Leader Institute. Jin is a 4th year medical student at Boston University. As a scholarship winner, Md. Jin will participate in a year-long leadership development program.
The Family Medicine Leads Emerging Leader Institute is a program of the American Academy of Family Physicians Foundation. It is funded by family physician donors and aims to identify and train Family Medicine residents and medical students who have leadership potential, but may not yet have served in a major leadership role.
Check out the article “Patients Cared For By Female Doctors Fare Better” written by Sarah Anne Schumann from DFM’s first residency class. Click here to read the full story.
DFM’s Holiday Party at the House of Blues was a great success! Click here to watch our fun montage of photos put together by our very own Doria from the holiday party. Thank you, Doria!
Congratulations to Katherine Gergen Barnett for being mentioned in the article “Restored Health Renews Purpose for Elizabeth”. Click here to read the full story.

Congratulations to Paula Gardiner, MD, MPH for her published article “Current State of Child Health in Rural America: How Context Shapes Children’s Health”.
This purpose of this essay is to provide a detailed description of the status of children in rural America to highlight features of the rural environment that may affect health. Click here to read the full article.
 Relational Practices in Health and Healthcare: Healing through Collaboration
Relational Practices in Health and Healthcare: Healing through Collaboration
By: Katherine Gergen Barnett, MD
What does relational health and healthcare mean to you?
Health in healthcare cannot happen without the power of the relationship. Traditionally, this has been about the connection between the provider and patient. Developing this relationship is a timeless art – one that is built on fostering curiosity, true listening, empathy, and understanding. Many of us spend our lives teaching these skills to medical students, residents and practicing doctors. However, in our increasingly complex world of medicine, relational health is beyond the matrix of the clinician- patient and spans to include relationship to other patients, relationships to other providers on the medical team, and relationships to community resources. Medicine is now moving to team based care where we have social workers, psychiatrists, pharmacists, nurse practitioners, practice assistants, nurses, patient navigators and care management members on our teams. Each of these individuals serves a critical role in bringing a patient to health. Group medical visits give a chance for patients to connect to others suffering from the same conditions and those relationships are part of their healing. Finally, health is created and strengthened when individuals are connected to resources within their community- getting locally sources foods at CSAs (Community Supported Agriculture) , exercising at the local Y, walking on safe sidewalks, biking in safe bike lanes, having safe affordable child care, etc. Healthcare is moving in a very exciting direction where increasingly we are getting government incentives to turn health care delivery in a much more relational way. This is what gets me excited every day in the work at Boston Medical Center, New England’s largest safety net hospital.
Click here to go to the website.
Congratulations to Suzanne Mitchell for being quoted in the Kaiser Health News story “How to Fight for Yourself at the Hospital- And Avoid Readmission” (click here to read the full story) and in the Daily Herald in the story “Don’t leave the hospital until you know comes next” (click here to read the full story).
.
Click here to read the full story.

Alysa Veidis
Associate Medical Director, Family Medicine at Boston Medical Center
Alysa Veidis, MSN, RN, FNP-BC, has been appointed by MA Governor Charlie Baker to serve on a special commission examining the feasibility of establishing a pain management access prive treatment options.
Click here to see this story in the Boston Business Journal.
Check out Katherine Gergen Barnett in the BMC Video “Patience Experience Forum: Improvements”
Chair Column April 26, 2016
To the DFM Faculty, Residents, Staff and Friends of the Department,
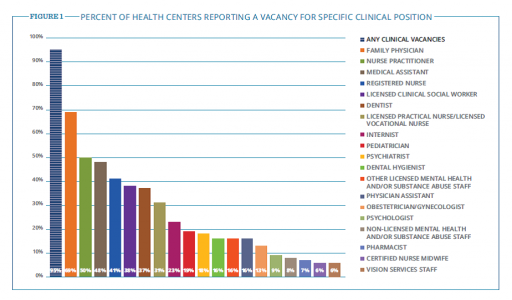
In this edition of the DFM Newsletter, I would like to highlight the value of our relationship with the Boston HealthNet Community Health Centers. CHCs are an important part of health reform. Across the US, 1,400 CHCs create a safety net for over 24 million patients. But challenges remain. Manny Lopes, CEO of East Boston Neighborhood Health Center points out at a recent National Association of CHCs (NACHC) meeting that recruitment and retention of clinical providers remains an issue.
Click here to read a supporting article:
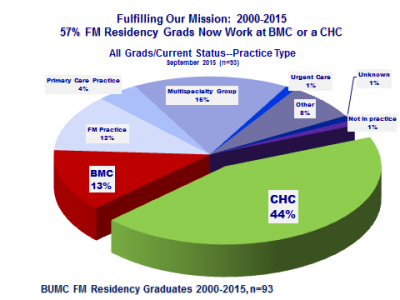
The March issue the NACHC newsletter reports that almost all health Centers (95%) are experiencing at least one clinical vacancy today. The positions that CHCs report to be most commonly vacant are those for family physicians. More than two-thirds of health centers indicate that they are currently recruiting for at least one family physician!
Our Boston HealthNet–BU Department of Family Medicine collaborative is working together to successfully recruit to our CHCs the kind of doctors America needs. I am proud to report that 6 of the 10 of residents in our graduating class this year are staying within the Boston HealthNet CHCs this year. They will be working at Mattapan CHC (2), South End CHC, Codman Square CHC, East Boston NHC, and BMC FM. Over the past 16 years, now 60% of all our 103 graduates have chosen to work in the BHN CHCs or in the DFM [link to the slide below] and the retention of these graduates is remarkably high.
Finally, elsewhere in this edition of the newsletter is an announcement of the first year residents who will be joining our program in June. You will notice that we now have expanded to 12 residents per year – and we are very proud that this group of newly matched BMC Family Residents — who are 50% underrepresented minority students – begin to looks like the community we serve.
By these measures, this is the most successful teaching CHC – academic health center alliance in the US – benefiting the people of Boston. This is something for which we should all be proud.
-Dr. Brian Jack

Hilton Minneapolis Downtown
Minneapolis, Minnesota
April 30-May 4, 2016
Presentation schedule: DFM Brochure STFM Annual_42116
Coming of the Light: The 2015 Integrator Top 10 for Policy and Action in Integrative Health and Medicine
#3. Katherine Gergen-Barnett, M.D. and Integrative Medicine Group Visits at Health Affairs
“Meanwhile, at the safety net Boston Medical Center, Katherine Gergen-Barnett, M.D. (pictured), a researcher associated with Paula Gardiner, M.D., MPH’s PCORI grant on integrative medicine group visits, broke through a rarely-crossed publication barrier with a paper on integrative medicine group visits in the powerfulHealth Affairs. It is long-past time to put these group-delivered services into the center of integrative education and practice.”
To read the full story click here.
Ground-Breaking Research on Integrative Medicine that may Help People Living with Chronic Pain
Transcription
Health Professional Radio
Wayne Bucklar: You’re listening to Health Professional Radio with Wayne Bucklar. My guest today joins us from Melbourne, Australia where she is visiting from Boston in the United States. It’s Dr. Katherine Gergen Barnett and she is the Director of the Integrative Medicine Clinical Services at Boston Medical Center. Katherine’s first trip to Australia, welcome to Australia Katherine.
Dr. Katherine Gergen Barnett: Thank you so much Wayne. I’m so thrilled to be here. And thank you for having me today.
W: Now I understand you’re here as the keynote speaker for this year’s Blackmores Institute Symposium, which is this week I think?
K: That is correct, yeah. The Blackmores Institute Symposium is this weekend and I’ve been very honored to present to them some of my research my colleagues and I are doing at Boston Medical Center on the treatment of chronic pain.
W: Now Katherine integrative medicine is not something I’m familiar with, but that’s not unusual because I’m not much of a clinician at all I’m afraid. Is that what you’re going to be talking about?
K: So let me just backup by saying you’re not alone and knowing so much about integrative medicine is a new in some ways a new field but certainly a growing field although it really draws upon many ancient traditions. Some of which are in the instance of traditional Chinese medicine over 2000 years old. So it’s really a study of medicine and a practice of medicine that brings in evidence based modalities both in the western medicine tradition such as pharmaceutical, surgery etc., as well from the other traditions such as “Ayurveda and traditional Chinese medicine and some Indian medicine.” Really to bring health and wellness to our patients in safe and effective means. And what I will be speaking about the conference during the keynote is really some of where we’ve gotten our current state of medicine today which is very much as we all know for anybody who has either been a patient or a practitioner, one that is largely burdened by chronic illness. WHO has put out many reports recently showing that the rates of Communicable Disease, ones that we’ve known for a long time are happily declining worldwide but our rates of chronic illness are going up at a rapid cliff. And the way that we have practiced medicine in traditional western medicine is excellent in so many ways and has really been a God sent in terms of treatment for communicable diseases, but in terms of treatment of chronic illness we know that we actually lack some of the tools to help people in a true kind of underlying way, and not just treating the symptoms but looking at some of the causes that maybe going on for some of the chronic illnesses and addressing those things. And again it’s no fault of any practitioner, that’s the way our system is set up. But an integrate medicine we’re really looking at mind body, spirit and how we can use all three of these things to get the person to propel to greater wellness.
W: Now Katherine as soon as you mentioned spirit, in many clinical circles it’s a degree of cynicism – your work is research based I understand?
K: Yes, yes thank you for clarifying. Yes, it’s everything we do is based on evidence in medicine. We’re very heavy research based group, we have grants from the NIH and from Federal Funding and what we’re doing in terms of your “spiritual” really looking at something called “mindfulness.” We just had a tremendous amount of literature and research behind it in terms of looking at some of these efficacies within chronic pain, and depression, cardiovascular disease. But really what we’re doing is again integrating those modalities into a larger medical setting. And so for instance with our care for people with chronic pain which is one of the main focuses of my talks at Blackmores Institute as speaker, we’re looking at how we can treat people with chronic pain using some of the integrative medicine approaches, but also really be looking at other thing such as you know –are there nutritional deficiencies that happening with our patients. Are there ways that we can kind a both through their health through things such as making inflammatory diet? Can we bring in their primary care physicians to treat them with different kinds of medication? And are we able to decrease some of their sequelae of chronic pain, such as depression by being in a group visit setting? Such as that they get support from other patients who are suffering from chronic pain and they know that they’re not alone and that actually goes a long way in decreasing their pain and suffering.
W: Now Katherine just for some of our audience who are not familiar with the American system, NIH that’s the funding body you mentioned, what is that body?
K: So that’s the National Institute of Health. That’s very well regarded collection of researchers based down in Maryland the Washington DC area that has the largest amount of federal dollar funding. And they give a number of grants through they have many different kind of branches study and they’ve given number of grants and scope procedures to get grants from them. And they’ve done tremendous work in advancing the research field on all levels of medicine.
W: Thank you for clarifying that for me.
K: Yes, thank you.
W: Given that you’re here talking about your research in pain management through this integrative approach, I assumed you’ve got some results that are fairly positive.
K: Yes, thank you for asking. So we’ve actually our group, our approach to chronic pain is called “Integrative Medicine Group Visits.” And the setup is such that a patient meet for 9 weeks in a group of up to 12 patients for 2 and half hours per session. And in that time as I shared with you many different modalities and the first set of data that we got after several years of running the group is that we had enormous reduction in pain, symptomatology we had reductions in depression, we had improvements complete, we had a reduction in perceived stress. And so our results were able to carry us forward into earning a very prestigious grant, again federally funded something called PCORI which is a patient center grant that Obama and this Affordable Care Act they are very focused on patient centered outcome. They granted us a $1.8 Million grant and look at our standard of care versus our intervention, and to see what the comparison was for our intervention with this standard of care for our patients. And so we’re currently 2 years into that study and that we haven’t published the outcomes, it’s continuing to be very exciting, very assurance in terms of the reductions in a lot of the most bothersome symptoms for people.
W: You’re listening to Health Professional Radio, my name is Wayne Bucklar. And my guest today is Dr. Katherine Gergen Barnett. Katherine is the Director of the Integrated Medicine Clinical Services at Boston Medical Center. And she is here in Australia to speak at the Blackmores Institute Symposium this week as the Keynote Speaker. Katherine many of our audience are clinicians, about 95% of them in fact are doctors, nurses, allied health professionals either in acute care or a lot in aged care. What message would you like them to take away from having heard you today?
K: So I just want us all to be able to think a little bit outside of the box in terms of taking care of our large numbers of people living with chronic pain. In Australia it’s 1 in 5 people below the age of 65. And once you get greater than 65, it’s 1 in 3 and these are very parallel in the US. And through the messages of speaking about the whole person in what you can do to improve not only treat their symptom of pain but perhaps get a little bit deeper into some of the causes of their pain. And it’s not all about fixing but rather sometimes it’s about doing, some of those causes.
W: Getting clinicians to think outside of the box is never a quick process into the health industry.
K: (giggle)
W: But I’m sure there’ll be some who’d be very interested to hear what you have to say and what you’d be saying on the weekend. Is there a common misconception about your work that drive you nuts and keep you awake at night?
K: I wouldn’t say very much keeps me awake at night, since I have 3 young children and I work full time.
W: (Laugh)
K: But I will tell you that I think this is changing happily because of the quality of research that is being done in this field, including ours at Boston Medical Center and many others in the US and the Blackmores Institute here. But I think that for me it’s really making sure that we are putting together good studies, and that we’re publishing our study so that all of us as scientific clinicians can really work together and look at the evidence, wipe away some of our biases and really look at what’s best for the patient.
W: Well let’s hope today that we can address that misconception with perhaps just a few, but will do our best. Katherine it’s been a pleasure having you on with us today. Thank you for making the time available.
K: Thank you so much Wayne. It’s an honor to do this work and to speak with you today about it.
W: If you just joined us, you’ve just missed my conversation with Dr. Katherine Gergen-Barnett who’s here for the Blackmores Institute Symposium this weekend from her regular job as the Director of Integrative Medicine Clinical Services at Boston Medical Center obviously in the US. The good news however is that on our website we have a transcript of my conversation with Katherine, we also have an audio archive on both SoundCloud and YouTube so do head off to our website at www.hpr.fm. You can check at either the audio or the transcript. My name is Wayne Bucklar, you’re listening to Health Professional Radio.
To hear interview click here.
League Celebrates 50th Anniversary of Nation’s First Health Center; Looks to Future of Community-Based Health
Victoria Reggie Kennedy, Mayor Martin J. Walsh, and U.S. Representatives Stephen Lynch and Michael Capuano will join national and local leaders and community health advocates for a day-long symposium to commemorate the 50th anniversary of the founding of the nation’s first community health center at Columbia Point, and to look to the future. Now serving one in seven Massachusetts residents, the community health center movement laid the groundwork for national healthcare reform and has proven that high quality care and lower healthcare costs can be achieved together.
The symposium at the Edward M. Kennedy Institute for the Massachusetts Senate will feature panel discussions on the federal government’s role in the creation and growth of health centers, how community health centers changed the model and delivery of healthcare, and 21st century workforce strategies to recruit new talent and bridge the provider gap. It will also include a speaking program with special presentations to Victoria Reggie Kennedy, the Kraft family and to Dr. H. Jack Geiger, whose vision spurred the roots of a movement 50 years ago. – See more at: http://www.massleague.org/#sthash.AvpdaONh.dpuf
To read more click here.
Halloween Fun in East Boston!
Syn demics and Legislative Outreach
demics and Legislative Outreach
Society for Medical Anthropology
Bayla Ostrach (Boston U School of Medicine)
Ashley Houston (Boston U School of Medicine)
Merrill Singer (U Connecticut)
An Experiment in Educating Congress about the Health Effects of War
Syndemics and Legislative Outreach | Anthropology-News
We often think of long-term health effects of war in terms of a legacy of suffering for combatants and people directly affected by battlefield events. Less attention is paid to the ways that war increases the burden of disease among broader populations. Little research focuses on how government policies and defense strategies such as sanctions, embargoes, and destruction of infrastructure are inscribed on the bodies not only of those who survive, but also in the illness experiences of those living in countries shaped by war, decades later. Two of us published an article in the Annals of Anthropological Practice, “Syndemics of War: Malnutrition-Infectious Disease Interactions and the Unintended Health Consequences of Intentional War Policies,” (Ostrach & Singer 2012) drawing attention to a syndemic composed of war policies that produce interactions between malnutrition and infectious diseases, to increase the overall burden of disease. Identifying a syndemic requires examining multiple diseases or biological factors that additively interact under adverse social conditions, resulting in biological interactions that would likely not occur without structural factors, and that increase suffering (Singer 2014). Syndemics illuminate mutually reinforcing layers of suffering related to biomedical, behavioral, and other health conditions that occur within and because of adverse social conditions.
Beyond Medicine: The Road From Health Insurance To Health
Congratulations to Katherine Gergen-Barnett, M.D. on the publication of her piece entitled Beyond Medicine: The Road From Health Insurance to Health.
Now that as many as 6.4 million low- and middle-income Americans across 34 states have health insurance as a result of the Affordable Care Act, it’s worth asking this question: When does health insurance turn into actual health?
It’s a legitimate question because the impact of health insurance on health has been shown to be less impressive than we might wish. At least one study out of Massachusetts, for instance, hasdemonstrated reductions in mortality associated with insurance status, while other studies out of Oregon show only modest reductions in mental health disease burden. So how much health have we really gained nationwide from the ACA’s insurance expansion? It remains to be seen.
In the meantime, it may be time to turn our collective attention to a slightly different question: Where else in Americans’ lives might we find more substantive ways to improve health?
To read more click here.
The BUSM Medical Education Office is Seeking Clinical Faculty to Join the Inaugural Cohort of BUSM’s Academy of Medical Educators
| To: | BUSM Faculty |
| From: | Priya Garg, MD, Associate Dean of Medical Education |
| Date: | March 21, 2019 |
| Re: | Academy of Medical Educators (AMEs) |
The BUSM Medical Education Office is seeking clinical faculty to join the inaugural cohort of BUSM's Academy of Medical Educators (AMEs) to serve as core faculty in the re-designed M1 and M2 doctoring courses. The course design is primarily case-based small groups, standardized patients and skills training.
After required faculty development, AMEs will teach communication, physical exam and clinical reasoning skills and advise students in cohorts of 8, and observe mid- and end-of-year assessments one afternoon per week throughout the academic year, covering the full scope of practice students need to enter the clinical phase of the curriculum.
Academy Educators will be hired for 10% FTE starting July 1, 2019 at the rate of $170k for instructors/assistant $180k for associate, and $190k for full professors plus fringe. Ideal applicants are MD or equivalent faculty who are passionate about clinical medicine, teaching and mentoring students and supporting their professional development. Applicants should have experience teaching and mentoring medical students.
If interested, please send your CV and a statement describing your interest and experience in the teaching required for this role to Ms. Rebecca Halley at rlhalley@bu.edu by Monday, April 1.
Congratulations to Brian Penti and Joanne Timmons for their published article “The Role of the Physician When a Patient Discloses Intimate Partner Violence Perpetration: A Literature Review”.
 Click here reach the full article.
Click here reach the full article.
BMC Cancer Care Center
Please see below a letter from Bod David, the manager of Cancer Support Systems to BMC Social Workers to remind us all of the Cancer Support Programs BMC offers. Also please see the flyer that was attached.
Hello BMC Social Workers,
This is a reminder that the Cancer Support Programs office is offering free ongoing Bereavement Groups for patients and staff who have lost someone to cancer or other long-term or chronic illness. Please keep in mind when deaths occur amongst your patients (and family of fellow staff).
Best,
Bob
Manager, Cancer Support Programs
Boston Medical Center
FGH Building, 2nd Floor
820 Harrison Avenue
Boston, MA 02118
Tel. 617-638-7540
Fax 617-638-8512
Take advantage of BU’s Institutional Membership with the NCFDD
|
|
PLEASE SEE OUR LEAN and MEAN PHARM TEAM
Congratulations to Paula Gardiner and her co-authors in the DFM!
Congratulations to Paula Gardiner and her co-authors in the DFM -- Katherine Gergen Barnett, Brian Penti, Rob Saper, Pam Adelstein, Ivy Brackup, Christine Farrell-Riley, Lance Laird, and Suzanne Mitchell – for publication of their important article article “Design of the integrative medical group visits randomized control trial for underserved patients with chronic pain and depression” that was published in Contemporary Clinical Trials.
Click the link provided to read the full provider: Published IMGV RCT Methods Paper.
Congratulations to Jeff Markuns, MD, MEd for getting his article “Development and validation of the Vietnamese primary care assessment tool”published!
“Congratulations to Jeff Markuns MD MEd for publication of the important article “Development and validation of the Vietnamese primary care assessment tool” in which he and his colleagues adapted the PCAT Primary Care Assessment Tool for Vietnam. This work will allow formal assessment of the rapidly growing family medicine sector within Vietnam that Jeff and his team have been so involved with for many years.
Click here to read the full article!
Nidhi Lal presented her narrative stories at the AAFP FMX 2017
Boston Student Selected for Family Medicine Leads Emerging Leader Institute Jin is one of 30 Participants
 Boston, MA- Helen Jin is one of just 30 scholarship winners nationwide selected to participate in he Family Medicine Leads Emerging Leader Institute. Jin is a 4th year medical student at Boston University. As a scholarship winner, Md. Jin will participate in a year-long leadership development program.
Boston, MA- Helen Jin is one of just 30 scholarship winners nationwide selected to participate in he Family Medicine Leads Emerging Leader Institute. Jin is a 4th year medical student at Boston University. As a scholarship winner, Md. Jin will participate in a year-long leadership development program.
The Family Medicine Leads Emerging Leader Institute is a program of the American Academy of Family Physicians Foundation. It is funded by family physician donors and aims to identify and train Family Medicine residents and medical students who have leadership potential, but may not yet have served in a major leadership role.
Click here to read the full story.
Family Physician Named as new BUSM Dean of Admissions
 I am pleased to announce the appointment of Kristen H. Goodell, MD, as Assistant Dean for Admissions at BUSM, effective Sept. 5. Dr. Goodell will become Associate Dean of Admissions upon Dr. Robert Witzberg's previously announced retirement (after 16 years in that role) on June 30, 2018.
I am pleased to announce the appointment of Kristen H. Goodell, MD, as Assistant Dean for Admissions at BUSM, effective Sept. 5. Dr. Goodell will become Associate Dean of Admissions upon Dr. Robert Witzberg's previously announced retirement (after 16 years in that role) on June 30, 2018.
In addition to her role in Admissions, Dr. Goodell will be an Assistant Professor of family medicine and an attending physician in family medicine at Boston Medical Center.
Dr. Goodell has served on Harvard Medical School's Admissions Committee since 2014. She also serves as Director of Medical Education and Co-Director of the Harvard Home for Family Medicine in Harvard Medical School's Center for Primary Care. In this role, she has developed and implemented educational programs in primary care and family medicine including the creation of new courses at all levels of medical education; from medical students through CME, with a particular focus on clinical skills, information mastery, and interprofessional education. Throughout her career Dr. Goodell has served as a mentor for medical students, particularly during points of career transition, as well as serving as faculty advisor for student organizations and committees. In addition, Dr. Goodell has served as the School Physician for the City of Medford since 2008 and a family physician at Winchester Physician Associates since 2007.
Dr. Goodell received her bachelor's degree from Colby College and her MD from Columbia University College of Physicians and Surgeons. She completed a residency in family medicine from the Tufts University Family Medicine Residency Program and a Tufts Master Teacher Fellowship from Tufts University School of Medicine.
Dr. Goodell is Chair of the national Council on Graduate Medical Education and Co-Chair of the Leadership Development Task Force of the Council on Academic Family Medicine. She is an ad hoc reviewer for the journals Academic Medicine, Family Medicine and Annals of Family Medicine. Dr. Goodell also served as a faculty consultant on medical education for the USAID-funded Health Advancement in Vietnam, and worked to address the oral health competency gap in primary care training with funding from the Health Resources and Services Administration (HRSA).
Dr. Goodell shares our dedication to the comprehensive and holistic admissions model and I am confident she will maintain and expand the successful, nationally respected program Dr. Witzburg has established. We will always be deeply committed to selecting and recruiting an exceptional and diverse student body.
I would like to thank the members of the committee for their work in developing a strong candidate pool and for their time for interviews and thoughtful discussion.
Please join me in welcoming Dr. Goodell to the BUSM and BU Medical Campus community