Bridge Builders
Doctors and Engineering Students Work Together to Build Innovative Devices
By Liz Sheeley
There can be a wide gap between new medical devices doctors need and the ones companies decide to make. This disconnect can leave doctors accepting something like a surgical instrument that hasn’t been redesigned in half century even when it can cause medical problems. Now, what started out as a year-long practical course for master’s students in Boston University’s biomedical engineering department, has turned into a way to help close that gap.
During their one-year program, all biomedical engineering master’s students must design and prototype a medical device to solve a problem they pinpoint while observing doctors at Boston Medical Center (BMC). Groups of students work with different medical specialists to formulate products that help patients and are feasible from an engineering, manufacturing, and budgetary standpoint. The drawback was the students’ graduation, which brought product development to a halt.
Seeking to continue the product development process over multiple years, Master Lecturer and Adjunct Professor Jonathan Rosen (BME) established The Bridge Builders Initiative in 2016. By employing enrolled master’s students who are also working on their own academic projects, alumni of the program, and undergraduates, Rosen put together a team to work with doctors at BMC and build trial-worthy products that could become marketable medical devices.
“I was excited because I thought, ‘Wow, these guys can create something that I need, but don’t have,’” recalls Dr. Alan Fujii, director of the Neonatal Intensive Care Unit at BMC. “Our babies are so small that there’s not so much room for error when we are doing procedures so I thought that the biomedical engineers could create stuff that would make working with neonatal babies easier and safer.”
John Subasic (BME ’16), along with three other graduate students, did just that. They designed an electronic pad that would take the vitals, including heart rate and blood oxygen level, of a premature baby faster than the standard method. It became the first Bridge Builders project.
“When a baby comes out and is respiratorily depressed, we have to figure out how depressed they are to administer the appropriate care and to do that we need to know the baby’s heart rate,” says Dr. Fujii. Right now, when a baby is born, doctors hold onto the umbilical cord’s stump and try to count out the heart rate, which can be tricky for even seasoned doctors. But using electrodes to read blood oxygen saturation rate and heart rate can also be a tricky process with neonates because the saturation monitor must be positioned exactly right on the infant’s foot to get an accurate reading. If the monitor reads zero, it can be difficult to know whether the monitor isn’t attached correctly or if the baby does not have a heartbeat. The hope is that a “smart” pad would remove the need to struggle with electrode placement and cut down on the time it takes for doctors to evaluate their newborn patients and get them the care they need faster.
Michaela Trexler (BME ’16, BME ’17) was among the first master’s students Rosen hired to work with Bridge Builders after she graduated and she continues to work with the program as an alumna. In addition, the Initiative hired undergraduate seniors to use their senior design project to help tweak the design of the pad over the next year. In August of 2017, the team celebrated its first success when BMC approved their proposal for a small, first-round clinical trial of the pad to evaluate its efficacy and accuracy.
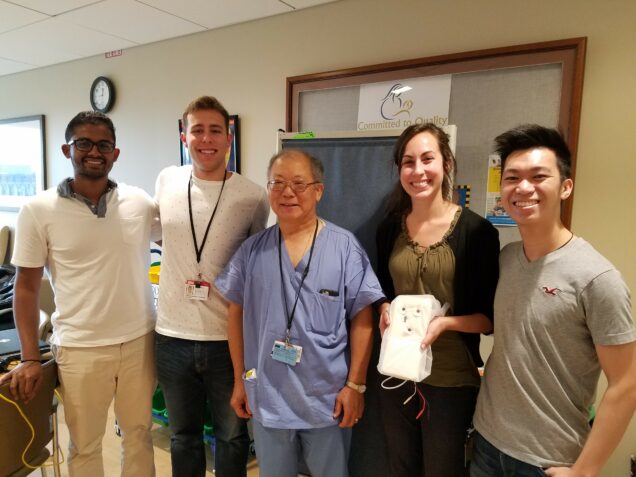
During the trial, the team found that wiggling infants can make it more difficult to get fast and accurate readings. To keep the babies in better contact with the pad, the team has proposed tweaking the design by rounding it up slightly, said Nicholas Leung (BME ’17), who was hired to coordinate the current students.
The smart vitals pad is just one of four Bridge Builders projects. The second project is a new surgical instrument Trexler helped design that spreads a patient’s rib cage during heart surgery. Standard, hand-cranked retractors exert force at an unnatural angle, sometimes cracking the patient’s ribs. The new internal mammary artery retractor, developed at BU, works with the body’s physiology by moving the ribs upward in a clam-shell like fashion instead of pushing them to the side.
“Not that opening your rib cage is ever natural,” says Trexler. “But if you have to do it, you’d want something that moves with the muscles and bones rather than pulling up at an awkward, harsh angle.”
Instead of handing students a problem to solve, the master of biomedical engineering program at BU gives students the opportunity to observe physicians in practice and work with them to conceptualize and prototype a solution to a real clinical problem. This hand-in-hand work is rare for a master-level program.
“We focus on how medical devices are designed and how those designs can lead to improved patient care rather than just teaching principles of design,” says Rosen.
“It’s really amazing because if you create something that that doctors find really helpful and that has a lot of potential, your idea has the possibility of becoming a full device,” says Leung. “That’s the whole goal of the Bridge Builder Initiative and is why I came to BU.”