Single-dose drug delivery system creates hope for streamlined cancer treatment
By Liz Sheeley
Chemotherapy patients experience visible and invisible side effects from treatment. Most common chemotherapy drugs must be dissolved in toxic chemicals to be administered intravenously, and they not only cause hair loss, the hallmark chemotherapy side effect, but they can also wreak havoc on the whole body by harming major organs and weakening the immune system. These drugs must also be administered over multiple sessions in order to allow the patient to rebound from the toxicity of the drug, and often require patients to get long-term catheters and return to the hospital multiple times.
An interdisciplinary team of biomedical engineers, chemists, and clinicians led by Professor Mark Grinstaff (BME, MSE) has developed a novel sustained-release, biodegradable nanoparticle system that carries a common cancer drug to deliver a therapeutic dose in one injection that has the same curative effect as the standard multi-dose effect. Essentially, this system could offer an alternative that is both safer for the patient and also improves quality of life by reducing adverse effects and eliminating multiple drug administrations. Their work, done in collaboration with Brigham and Women’s Hospital and the University of North Carolina at Greensboro, has been published in Chemical Science, a Royal Society of Chemistry journal.
The chemotherapy drug used in this research, paclitaxel (PTX), is commonly used to treat lung, breast and abdominal cancers. To be used for treatment, PTX must be dissolved in a specific chemical variation of castor oil, which is known to cause severe allergic reactions and neural toxicity. In addition, it is difficult to give high doses of PTX because there is a fine line between a therapeutic dose and a toxic dose. To overcome dosing complications, doctors have tried to treat those abdominal cancers locally, but unfortunately, patients commonly experience catheter-related complications and toxicities that ultimately limit the total number of doses a patient receives.
Nanoparticles offer a safe delivery system for chemotherapy drugs like PTX with only a single dose. There are many different types of nanoparticle systems in development. They work by encapsulating the drug in a large molecule known as a polymer, and scientists can vary type of drug, polymer, and chemical bond used in the system. These systems provide doctors the opportunity to safely give their patients a single higher dose of chemotherapy drugs and remove the need to use the toxic carrier or more invasive administration techniques, which could reduce adverse side effects and improve quality of life.
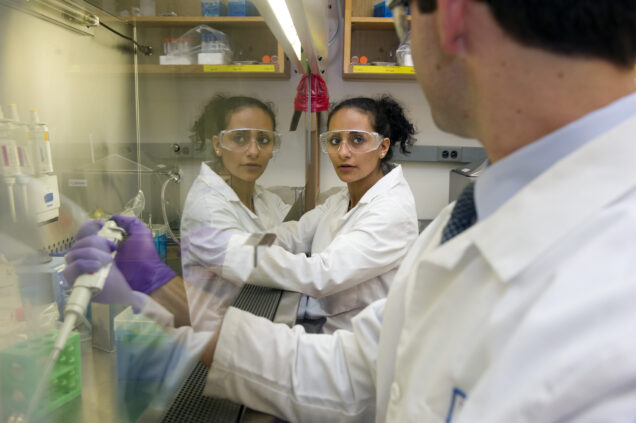
Iriny Ekladious, a BME graduate student in Grinstaff’s lab, said their team decided to use a novel polymer that was developed in the Grinstaff lab in 2015, and use a chemical bond that breaks apart in the presence of water to link the drug to the polymer. Many researchers have observed that cancerous cells take up more nanoparticles than normal cells and the same phenomenon occurred with this nanoparticle system. Their novel approach provides another potential mechanism that could reduce the severity of current chemotherapy side effects because less drug is circulating in non-cancerous regions of the body. The degradable and safe polymer used in this research is hydrophobic, or water repelling, which causes the bonds between the polymer and the drug to slowly break and creates a sustained, slow release of the drug.
Since confirming that the single-dose delivery system is just as effective as the traditional multi-dose chemotherapy delivery, researchers can now tweak the system. These tweaks could be trying a new way to bond the drug to the polymer, or developing a chemical that could trigger the release of the drug from the polymer.