Damiano’s concern was appropriate. Dead-in-bed syndrome, which takes the lives of the 6 percent of people with type 1 diabetes who die before the age of 40,
is a bogeyman that haunts every parent of a child with diabetes. His background in biomedical
engineering did
not exempt him from the dread.
Next, Damiano, a College of Engineering associate
professor of biomedical engineering, would do a quick
blood stick in one of David’s fingers or toes, draw some
blood into a test strip, and wait for the glucose meter
to return a number. If the number were too high, or
rising too fast, he would give insulin; if it were low, or
dropping too fast, he would wake his son and give him
juice or lower the insulin infusion rate, or both. Then he
would go back to sleep for two or three more hours.
Type 1 diabetes, which affects about two million people
in the United States, is an autoimmune disease that destroys
the pancreatic cells that normally produce insulin, a hormone that allows the body to convert carbohydrates
to energy. Instead of being put to
work by muscles, the sugars build up in the blood,
creating a toxic combination that if treated poorly
over many years is almost certain to damage organs
such as the kidneys and eyes, as well as blood
vessels and nerves. The consequences before the
discovery of insulin 90 years ago were even more
dire: without the ability to draw upon the sugar in
the blood, the body would inevitably waste away
and starve to death.
View Video
Video
Developing the Bionic Pancreas
By Taylor Toole
Ed Damiano and his family talk about living with type 1 diabetes and his effort to build a bionic pancreas.
David Damiano’s type 1 diabetes showed itself
at the extraordinarily young age of 11 months.
Toby Milgrome, David’s mother and a practicing
pediatrician, will never forget the experience.
“David had been a normal, happy little boy,” she
says. “He was learning to walk, pushing a wagon,
and then one week he just seemed to be tired. He
didn’t want to get up; he was refusing to walk. At
the end of the week he was just kind of staring
into space.”
Milgrome took David to see one of her pediatric
partners and requested some blood tests.
“I had a few things in my mind,” she says. “I was
thinking diabetes, leukemia, and brain cancer, but
I was hoping for nothing. I was hoping my partner
would tell me that there was nothing wrong.”
Hours later, the family learned that David
was suffering from ketoacidosis, a symptom of
diabetes. His extremely high blood glucose level
was nearly 10 times what it should have been.
They went straight to the hospital, where David
was admitted to intensive care.
Close
Ed Damiano talks about the challenges of treating children with type 1 diabetes.
 View Video
View Video
David’s parents knew little about living
with type 1 diabetes, but they learned fast. One
of the first things they learned was that the
available medical expertise was frustratingly limited. After disagreements with more than
one endocrinologist about the best treatment,
Milgrome and Damiano decided to put their son
on an insulin pump, a disposable battery-operated
device the size of a pocket watch that delivered
relatively precise injections of insulin under the skin. The technology had been available for about
10 years for adults, and most physicians were not
yet persuaded that it was suitable for use with
very young children.
“Now they will put little children on pumps,”
says Milgrome. “But the way they usually managed
kids was, they’d get a couple of shots a day
and their blood sugar would run around 180 to
250 mg/dl. The kids live and they have a life, but
we weren’t comfortable with that because of what
we know about long-term complications. Some
people said, ‘Don’t worry about it. He won’t get
any complications for 20 years.’ But in 20 years,
David would be only 21.”
Close
David’s mother, pediatrician Toby Milgrome, explains how David’s physical activity impacts his blood sugar.
 View Video
View Video
They also learned why there was little consensus
about the best ways to maintain a healthy
blood sugar count (between 70 and 120 mg/dl
in people without diabetes): it’s extremely hard
to do. Without a functioning pancreas to keep
things in balance, the amount of sugar in a person’s
blood climbs and dives in response to
a variety of stimuli, such as the amount and
intensity of a person’s physical activity, state of
mind, illness, stress, and many other factors, not
to mention the hormonal changes of a growing
child. An insulin dose that works fine one day may
be ineffective or excessive the next day. Insulin
dosing is an art form, Damiano says, and any given
dose often defies simple prescriptive regimens.
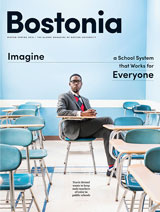
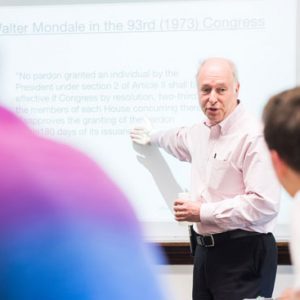
 Damiano’s aim in building a bionic pancreas for people with type 1 diabetes is to remove the human brain from the equation. An algorithm might work better, and certainly more consistently. Photo by Cydney Scott
Damiano’s aim in building a bionic pancreas for people with type 1 diabetes is to remove the human brain from the equation. An algorithm might work better, and certainly more consistently. Photo by Cydney Scott
An Exquisite Piece of Biological Machinery
Close
Toby Milgrome explains what a bionic pancreas means to people with type 1 diabetes.
 View Video
View Video
Damiano’s expertise had been in the application
of fluid dynamics and solid mechanics
to physiological systems. He spent years
doing mathematical analyses of blood flow in
microcirculation and the fluid dynamics of
the inner ear. But he is also an engineer, and
engineers design systems to solve problems. In
2004, when David was five years old, Damiano
set to work on something he knew he had to do:building a bionic pancreas.
He describes the natural pancreas as an exquisite
piece of biological machinery, one that fine-tunes
a body’s glucose level both by lowering it
(with minute amounts of insulin) and by raising
it (with another hormone called glucagon). The
real thing has many advantages that the manmade
technologies now available cannot rival. For
one thing, says Damiano, the pancreas releases
its insulin and glucagon directly into the liver,
where they can get to work immediately. Insulin infusions under the skin with an insulin pump can
take an hour or more to reach peak absorption.
But for Damiano, one of the most compelling
advantages of a natural pancreas has as much to
do with constancy as efficiency—a real pancreas
is relentless—it works while you’re awake and it
works while you sleep.
“Sleeping is the scariest part of all this,” he
says. “It’s what put this project on a high-speed
rail. It’s a very scary prospect that blood sugars
could go low at night. When you’re sleeping,
you’re checked out—you don’t want to check
out permanently.”
Jeff Hitchcock, the founder of Children with
Diabetes, an online community promoting a
better understanding of the care and treatment
of the disease, shares a parenting history with
Damiano. His daughter’s type 1 diabetes emerged
when she was 24 months old.
“Whatever you do in a life with type 1 diabetes
is impacted by that diabetes,” says Hitchcock.
“Every morsel of food you eat, you think about it.
Every time you go to sleep you think about it.”
Close
David Damiano talks about learning to check and regulate his blood sugar.
 View Video
View Video
Insulin dosing is normally done with extreme
care, by the person with diabetes or by a guardian.
For years, for example, Milgrome has been preparing
David’s meals and snacks for school, and
with each meal she includes a card detailing
the carbohydrate content and insulin dose. She
has also prepared a chart with insulin doses
to be given for high blood sugar. But no chart
can account for everything that might affect a
young child’s blood sugar from day to day. As
an additional measure, the nurse in David’s elementary
school would call either Milgrome or
Damiano five times throughout the day
and read them their son’s glucose levels;
they would then recommend an insulin
dosage that may depart from the standard
dose regimen, depending on a variety of other
factors that needed to be considered.
Damiano wanted to remove the human
brain from the equation. If a human could do
it, he reasoned, an algorithm could do it, and
it could possibly do it better, and certainly
more consistently.
When you’re sleeping, you’re checked out. You don’t want to check out permanently.
He envisioned a bionic pancreas as a trio of
connected devices: a continuous glucose sensor,
which could be worn on one side of the body
just above the waist, a dual insulin and glucagon
pump, which could be worn on the other side of
the body, and a small computer, which could be
built into the pump and would determine how
much insulin or glucagon to administer.
By 2008, three companies in the United States
were marketing continuous
glucose monitors, a golf-ball-sized
device with a sensor
placed just under the skin of
the abdomen that measures glucose levels every
five minutes. Before that, people with type 1 diabetes
managed their blood glucose levels with an
insulin pump. Today, about one in four people
with type 1 diabetes wears an insulin pump. The
missing link has been a mathematical solution,
an algorithm that would run on a computer
or smartphone, analyzing glucose levels and
determining how much insulin or glucagon the
pump should administer.
“In the current embodiment of our system,”
says Damiano, “glucose levels stream from a small
sensor/transmitter unit worn by the person into a
receiver, and the receiver then passes data into an
iPhone, where an app with our algorithm makes
a therapeutic decision to dose either insulin or
glucagon, with two small infusion pumps, every
five minutes.”
Most important, the algorithm could do it
while the wearer of the bionic pancreas sleeps,
eliminating, at least in theory, dead-in-bed
syndrome. Damiano knew exactly what he had
to do, and he knew when he wanted it done:
by fall 2017, when David would be heading
off to college.
 In a clinical
trial at MGH,
11 adults with
type 1 diabetes
were hooked
to the first-generation
version
of Damiano’s
system for 27
hours and were
supplied with
three high-carb
meals. Photo by Ed Damiano
In a clinical
trial at MGH,
11 adults with
type 1 diabetes
were hooked
to the first-generation
version
of Damiano’s
system for 27
hours and were
supplied with
three high-carb
meals. Photo by Ed Damiano
From Pigs to Humans
Close
Ed Damiano and research partner Firas El-Khatib talk about how they work together.
 View Video
View Video
Working with Firas El-Khatib, an ENG senior
research associate, Damiano started
experimenting with pigs in 2005. Their first
hurdle was fine-tuning the algorithm to churn
out immediate and precise responses to the wild
fluctuations of sugar in the pigs’ blood.
In spring 2006, Damiano gave a talk about
their work at the Joslin Diabetes Center in
Boston. When he left the
podium, he was approached
by Steven Russell, a physician
and researcher at Massachusetts
General Hospital
(MGH), who understood
the implications of the research.
Russell said he wanted
to help bring the technology
to humans.
In 2008, with assistance
from the Wallace H. Coulter
Foundation, the Juvenile
Diabetes Research Foundation,
the Helmsley Charitable Trust,
and the National Institutes of
Health, Damiano, El-Khatib,
and Russell began a series of
human trials. In the first of
these, 11 study subjects stayed
in a hospital room with an IV in
each arm for one day and one
night and ate three high-carb
meals. The first-generation
version of the system controlled
the subjects’ blood glucose for
27 continuous hours and used
blood glucose sampled from one
of the IVs as the input signal to
the control system.
A second study, launched in 2010, used the
second-generation version of the system, which
relied on glucose levels sampled from a continuous
glucose monitor placed just under the skin.
Subjects spent two days in the hospital and had
their glucose controlled for 51 continuous hours,
eating six meals and doing the kind of light exercise
that would send their glucose downward.
A third study, conducted last fall, validated the
performance of the second-generation system,
which had been modified to accommodate both
adults and adolescents. In that study, 12 adults
and 12 adolescents followed the same protocol
as in the second study.
The main goal is to get something in David’s hands before he leaves for college.
One of the greatest challenges the researchers
faced in developing their mathematical algorithms
was devising a single system that could
quickly and automatically adapt to meet the
vastly higher insulin requirements of adolescents
while at the same time not overdosing with too
much insulin when determining the much lower
insulin needs of adults.
Close
Ed Damiano talks about the scope and success of a recent outpatient study.
 View Video
View Video
This past February, Damiano and his colleagues
got approval from the MGH Institutional
Review Board to conduct their first
outpatient study with the current iPhone-driven
version of their bionic pancreas.
“Previous systems we designed all ran on a
laptop computer,” Damiano says. “It hung on
an IV pole, and there was a large contraption
you had to pull around if you wanted to ambulate
up and down the hallway. In lieu of this, we
built the whole device into an iPhone platform,
using a custom app that incorporates all the
mathematics. We’ve built a user interface with
the help of some of the folks at Information
Services & Technology at BU, so there’s a nice
graphical user interface that allows us to control
the system and visualize real-time glucose levels.”
Because the system uses an iPhone, Damiano
and El-Khatib could use the cellular network and
a cloud-based service to view each experiment
remotely on iPhones and iPads. They could also
review every subject’s real-time glucose levels
and all insulin and glucagon doses given to the
subject by the device.
Close
Ed Damiano talks about making blood sugar information accessible by iPhone.
 View Video
View Video
In their latest trial, 30 adult subjects wore
the device for five days and five nights and were
free to wander, iPhones in their pockets, around
a three-square-mile area in Boston by day and
sleep in a hotel next to MGH by night. Next,
Damiano says, he will conduct a study in 32
children who will wear the device for five days
and five nights in a diabetes summer camp in
central Massachusetts.
 An iPhone displays a patient’s blood sugar levels and runs an algorithm that determines insulin needs.
An iPhone displays a patient’s blood sugar levels and runs an algorithm that determines insulin needs.
The final study with an iPhone, scheduled for
the first half of next year, will involve 48 adult
subjects wearing the device at work and while
sleeping at home for 12 days and 12 nights. In
2015, Damiano plans to conduct what he calls
the pivotal studies, which will test the commercial product that he plans to build over the
next 18 to 24 months. That product, he says,
will embed all of the functionality of the
current investigational device in a single
dual-chamber pump.
Close
Firas El-Khatib and Ed Damiano are in near-constant communication.
 View Video
View Video
“In the study’s final form, people with type 1 diabetes from across the country will wear the device for six months or so,” he says. “We’ll compare the glucose control our device was able to achieve in that cohort with the control a similar cohort was able to achieve when managing their own diabetes with their usual care over the same period of time. Our goal is to do those pivotal
studies in 2015 so that we can submit the device to the Food and Drug Administration for review the next year, and hope for approval by 2017.
That’s the goal—to get this done in about four
years’ time. It’s very ambitious, but I think we
can stay on track.”
Hitchcock believes that Damiano’s device will
“remove the albatross that circles above everyone
with diabetes” and will fundamentally change
life with diabetes. “It will free you from constant
mathematics every time you eat,” he says. “It will
free parents from fear every day that their child
will die every time the child goes to sleep. What
Ed is doing is going to change the world.”
Close
David talks about living with an insulin pump.
 View Video
View Video
David, who is now an active eighth grader
with a highly accurate jump shot, is, unsurprisingly,
his father’s number one fan. “I know it’s
really tough,” he says. “He’s been working on this
for so many years. I know his motivation is me,
but I know it’s more than me. It’s everyone with
type 1 diabetes, and I think it’s really great. I’m
really proud of him.”
“When we started this project, we were definitely
focused on trying to build something that
can take care of everyone with type 1 diabetes,”
says Damiano. “But my main goal was also to
get something in David’s hands by the time he
leaves for college. That’s really why I’m doing
this. I’m not particularly interested in glucose
levels in people’s blood. It’s not an interesting
thing to think about, but I have to think about
it all of the time. It shouldn’t have to be that way.
Ideally, no one should have to concern themselves
with it, ever.”
Ed Damiano’s bionic pancreas would free patients from much of the uncertainty involved in dosing.
Type 1 Diabetes
Healthy cells in the presence of insulin
Insulin produced by the pancreas binds to receptors on cells throughout the body, signaling the cells to absorb glucose from the bloodstream. Cells convert the glucose into energy.
Starving cells in the
absence of insulin
In type 1 diabetes, the
pancreas produces little or
no insulin. Without insulin,
cells are unable to absorb
glucose, and it builds up
dangerously in the blood.
Bionic Pancreas This version of Damiano’s system was used by patients in a study in February 2013.
Continuous glucose monitor measures glucose levels just under the skin and transmits the data wirelessly to an iPhone.
iPhone receives data and runs an app with an algorithm that computes insulin and glucagon doses.
Dual pump is commanded by iPhone to deliver insulin when glucose levels rise and glucagon when glucose levels fall.
Diagrams by Ed Wiederer




















































hi, we just descovered our child is diabetic, but for instance after having a breakfast without having insulin his sugar level was ok but after having a lunch it was high, so should my kid have insulin injevtion or not . please help me because in here in my city we dont have a good doctor and my kid penkerias seems working sometime . so what can i do?????
I am 42 years old and have had type 1 diabetes since I was 17. I have had a very tough time with it being what is labeled a “brittle” diabetic. When I read the article about David Damiano’s work in Time magazine, it made me tear up with the thoughts of having the most important and constant thing on my mind removed and my health increased. I pray this bionic pancreas comes sooner than later for it will truly change the treatment of diabetes forever.
My daughter was diagnosed with type 1 diabetes when she was 3 years old. She’s 22 years old now and she’s in her junior year in the college.
We live in Florida and she’s by herself in Philadelphia for the last 3 years. She’s so active, playing tennis, but her blood sugar is low and high sometimes. There is no word to describe how we lived since she was 3 years old and especially for the last three years. It’s been so difficult for me as a mom and every single second I’m thinking about her and worry. I can’t wait to see this new technology, bionic pancreas, in the near future.
I want to say thank you so much for all your efforts for doing this for all families who are suffering with type 1 diabetes.
God blasts you and your family!
Shadan
This is fantastic! I’m a 47 year old male who has suffered with type I diabetes since I was 17. I try to stay very active between exercise and playing ice hockey and really struggle to keep my blood sugars consistent even on an insulin pump.
This research and development you are involved with will change lives!
I know this must be exhausting for you and your family but keep the faith.
I would be interested in participating in the clinical trial and I’m sure you get requests all the time.
God Bless You and the work you’re doing to help others.
I’m 67 with type 2 for over 30 years. Talk daily with my cousin (retired neurosurgeon with type 2). We have frequently discussed the need for an implanted device to monitor and administer the disease. Interested in how the insulin and glycogen supplies are replenished.
I saw this notice and was very interesting for me. I have a son who have Glucogen Storage Desease. And, maybe in a future this new technology can help for this problem too.
Thanks for share and make something that is going to change the life for many people.
I´m a mother of a 15-year-old girl with diabetes type 1 from when she was 9. I really appreciate all your efforts to make people´s lives easier.
Thanks a million for your great dedication, and I hope all your work could reach one day to every corner of this world, as in my case. I live in Canary Islands (Spain).
Thank you indeed
Mari
Spain
I was diagnosed with Type 1 when I was 7 and I am now 58 years old. Two years ago I had a low BS during the night and fell and broke my collarbone. I suffer from low BS at night. I am thrilled to see this in our future, and would love to be a tester!! Will be following its progress. Thank you…..thank you……thank you!!
Ed Damiano
I am advanced type 2 diabetic, which has been steadily getting worse in last 2 decades, and take both insulin and glucagon. I take 2 types of insulin (short- and long-term insulin) for highs and glucagon for lows, with glucose tablets and juice if I am conscious and glucagon if very low or in a coma administered by my wife. I test and take insulin 8 to 10 times a day. I have had multiple comas with lowest with blood sugar measured in ambulance of 17 with direct injections of glucose. I test for 65 to 115 for waking test and 65 to 180 during the day. It would be a dream to have most of my readings between 70 and 120.
I read the Bloomberg article and the Boston University article.
It is the best news I have heard. While I live in south Florida, in St. Lucie County, I am not in the Boston area where the tests were conducted. BUT I WOULD BE A WILLING VOLUNTEER IF TESTS WERE DISTRIBUTED AROUND THE COUNTRY.
I WOULD BE WILLING TO COME TO BOSTON FOR TESTING FOR A PERIOD OF TIME.
I am a retired chief scientist with the FAA for GPS and navigation and worked on the NASA moon landings. I have worked for IBM, Hughes Aircraft, Fairchild Space, etc.
George Zerdian
My 41-year-old son’s pancreas was surgically removed in 2009. His blood sugars are very difficult to control and he has dangerous lows and highs even with an insulin pump.
If you need a tester in the Midwest (Iowa), I am sure he would gladly volunteer.
Keep up the good work. Time is of the essence for a lot of people.
Hello,
Both our daughters have type 1 diabetes. Our eldest is going to UC Davis for electrical engineering in the fall. We were hopeful to have a trained diabetic alert dog to go with her. Not to be so.
If you need another tester, we would be relieved if she could be one.
And UC Davis might like to help, too. They are involved with the contact lens Google is developing to measure blood sugar.
We just have the same concerns as you do, that our daughter will make that simple mistake, and not wake up.
Sir Ed Damiano, thanks a lot for the great news that will change the life of millions of people worldwide. My daughter is 12 years old and was diagnosed with type 1 diabetes 2 years ago.
I am a 62-year-old woman, living as a DT1, for 52 years.
Since I started with glass syringes, one had to boil before every use, the pump has improved my life considerably. But being classified as brittle, and I know there are many out there who say, “There is no such thing as a brittle diabetic,” control is difficult. I tried the continuous glucose monitoring system, but was continually bolusing or editing my basal
Hopefully, the bionic pancreas will make life better for us.
Judy
USA
I am 37 years old and have been Type 1 since 16 months old. I can attest to several of the comments that the current technology, while improving, still needs work. This new “bionic pancreas” study is what dreams are made of. My hats off to everyone involved, and I am looking forward to the public release. Thank you for all you are doing.
I`m 34 years old, living with DT1 for nearly 33 years. Waiting for decades…
I`m sure you will change the diabetes world.
God bless you
Rebecca
Germany
This definitely is brilliant for all the type 1 diabetics-a life without daily blood sugar tests and a fairly normal life! I do hope this study and approval could be expedited. Thank you for doing this.
What a well done story. Thank you.
It will be a great day for insulin-dependent diabetics when this is available.
Existing glucose monitoring devices and insulin pumps have problems when the infusion/monitoring sites have been in for too long a period of time. Infusion sites stop delivering insulin properly. Monitoring sites stop being able to read the glucose levels of the blood properly. What is being done about infusion/monitoring sites when they are no longer able to perform as they should?
I’m so happy to hear about this new technology. I’m 50 years old now, living with diabetes for 32 years. I struggle to manage my condition. I had laser eye surgery a number of times since 2005 and still have relatively good vision. I also have some diabetic-related kidney stress. I’m so scared facing the autumn and winter period of my life. Is there no way that this product can be released for public use at this stage of development? From what I have read, it appears to work well. Surely what is available now is much better than conventional management systems. It would make such a difference to people like me. There are people like myself whose health due to diabetic complications may have deteriorated significantly by 2017…we may not have the luxury of waiting that long. Please move process along as speedily as possible, and, if possible, release for public use what you have got now.
Gerry
Ireland
My best wishes for earliest successful completion and commercial availability of the product. My wife and daughter are diabetic. We live in India.
Recent graduate of BU School of Public Health– this was my first edition of Bostonia– so happy to find this on the cover!
Our daughter was diagnosed with Dt-1 in March. She is 14. It has been an incredibly difficult time, although we are adjusting. My copy of Bostonia arrived, and she said, “Look Mama! Someone in Boston is trying to help the kids with diabetes!” She read it aloud to me in the car as I drove. All I can say is THANK YOU so so much for trying to do this. You are a HERO! I formed a “SUGAR MAMAS” group of moms in my area with kids who have DT-1 and we ALL are afraid of the dead-in-bed syndrome. Not one of us sleeps anymore–2am wake up is the new normal.
Ed, you have no idea the hope you have raised in the town of Palos Verdes…please keep going…so all our kids here can ALSO have this by the time they go to college.
God Bless You
Dr Monica Westley (BUMC 1988)
I appreciate that the online article fixed the naming mishap on the Type I diabetes diagram (the print version has the titles for liver and stomach switched), but I would have hoped that an editor or someone would have caught that before the magazine went to print. Otherwise, a very informative article.
Absolutely brilliant. I am thrilled by literally everything about this story and how it is covered. Thank you!
As a BU MBA alum and type 1 diabetic, I was thrilled to see this cover story in my mailbox. Great work to everyone involved!
In type 1 diabetes, the beta cells of the pancreas are attacked by the immune system. The beta cells are the ones that produce insulin, however, the alpha cells, the ones that secrete glucagon, are not affected, so I’m having difficulty with why this “bionic pancreas” would secrete glucagon if your anatomical pancreas is still secreting it. Also, what about the delta cells, which secrete somatostatin, which reduces the rate at which nutrients are absorbed from the intestine, and the gamma cells, which secrete a pancreatic polypeptide to reduce appetite?
All in all, I think it’s a fantastic idea that may help take the angst out of the disorder that I have had for 28 years…
Michael,
My understanding is that we cannot count on our bodies to secrete glucagon. If we could, no diabetic would ever have a seizure from a low and there would be no “dead-in-bed”.
Prof Damiano is the man!