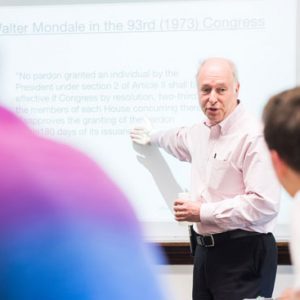
Tracy Battaglia was an undergraduate at BU studying psychology in 1990 and planning to begin medical school at the School of Medicine, when she was diagnosed with stage 4 lymphoma. “I had a positive experience with my treatment and did not encounter any delays in my care,” says Battaglia (CAS’92, MED’96, SPH’01). After completing her residency, she returned to BU in 1999 for a fellowship in general internal medicine and women’s health, and started seeing patients who had just been given a cancer diagnosis—or a potential cancer diagnosis—and many of them weren’t coming back for care.
“There were things in their way, and that really resonated with me,” says Battaglia, now director of MED’s Women’s Health Unit: Center of Excellence in Women’s Health and a practicing clinician in the Women’s Health Group clinic at Boston Medical Center (BMC). She was bothered by the dichotomy she saw between the city’s vast medical resources and this vulnerable patient group. “Boston has an embarrassment of riches, and yet we still had a population that was delaying care,” she says, and then she asked herself, “Why was that the case and what could we do to treat that critical disconnect?”
Battaglia, a MED associate professor of medicine, a School of Public Health associate professor of epidemiology, and director of medical education at BMC’s Belkin Breast Health Center, was sure there were things that could be done to improve the problem. “We did focus groups and key informant interviews, and we tried to understand what the challenges were for patients to come in. We found many, including a lack of coordination of services,” she says. “The system was so fragmented that patients were confused, and they had their own specific barriers to navigating the system.” Those ranged from lack of transportation and insurance to language barriers and sociocultural issues that breed fear and mistrust.
Teaming up with the Avon Foundation in 2001, Battaglia helped launch what was one of the country’s first patient navigation programs, where underserved breast cancer patients are paired with a “navigator” from the same neighborhood, or one who shares similar culture or language, to help deal with the numerous issues that could block the patient from timely care.
BMC’s early patient navigation program—initially called care coordination—was developed on the heels of a similar program launched by Harlem Hospital surgical oncologist Harold Freeman in New York City in 1990. Freeman had seen that women in medically underserved or minority communities had greater barriers to screening, diagnosis, and treatment than those with better access to care. With patient navigators helping these women overcome obstacles to care, he found, their outcomes changed markedly. At Harlem Hospital alone, the five-year survival rate jumped from 39 percent prior at the program’s start to 70 percent. BMC’s patient navigation program targeting underserved and minority women in Boston demonstrated a 12 percent improvement in mammography screening rates and a 15 percent improvement in timely follow-up rates after an abnormal screening test and helped reduce missed appointments at BMC by 50 percent.
Read the full story on BU Today






































Related Stories
Shipley Center Website Offers Prostate Cancer Facts for Patients
Gift from alum and trustee funds research and information warehouse
Too Many Black Women Die from Breast Cancer. Why?
BU Slone Epidemiology Center researchers look for answers
Zebrafish Cancer Genetics Illuminate Human Breast Cancers
MED’s Hui Feng focuses on MYC gene
Post Your Comment