The study was so explosive that an entire Harvard conference was convened to debunk it: research published last year concluding that being mildly obese does not shorten life span, while being slightly overweight actually could lengthen it.
Spearheaded by epidemiologist Katherine Flegal of the Centers for Disease Control and Prevention’s National Center for Health Statistics (NCHS), the research reviewed 97 weight studies covering almost three million people. It found that overweight people had lower death rates than people whose weight was normal and that mildly obese people didn’t die at greater rates than normal-weight people. Researchers call this counterintuitive conclusion the “obesity paradox.”
Skeptics cautioned that the normal-weight people in the study included smokers and some with serious illness and that those traits, not their weight, likely killed many of them and jacked up the mortality rate. A BU researcher says his work supports the skeptics.
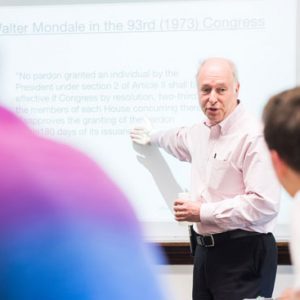
Andrew Stokes, a School of Public Health assistant professor of global health and a faculty member of the Center for Global Health & Development, researched the obesity paradox earlier this year while a graduate student at the University of Pennsylvania. Mining more than a decade’s worth of health surveys from the Centers for Disease Control and Prevention, Stokes cross-referenced that data with death records of American adults between the ages of 50 and 84. His finding, published in the journal Population Health Metrics: one-third of those deaths among nonsmoking Americans could be linked to excess weight or obesity.
“Much of the medical community actually believes that…at older ages and with medical conditions, extra weight sort of protects from fragility, buffers against the wasting associated with disease,” Stokes says. Flegal’s work in particular has credibility because of her employment at the NCHS. “People take it as official government statistics,” he says. But the obesity paradox is false, he argues, and he spoke with Bostonia about why his research, funded by the National Institutes of Health, reached different conclusions.
Bostonia: How did you go about investigating this?
Stokes: The vast majority of studies on this topic use body mass index at a single point in time, such as when they interview the subject. Using that weight and height at that point in time, they follow up with people for their health outcomes, comparing those who were obese at that single snapshot to those who were not obese. So the major innovation in my study is to incorporate weight histories into the analysis. All Flegal knows about her normal-weight subjects is that they have normal weight; what I know about my population is not only that they are normal weight, but what they were 5 to 10 years ago. For the people who got sick and lost a lot of weight, I can go back in time and identify their pre-illness weight.

Andrew Stokes says his work supports skeptics cautioning that normal-weight people in the Flegal study included smokers and some with serious illness, which likely jacked up the mortality rate. Photo courtesy of Stokes
Using the weight histories, you can disentangle people in the normal weight category who are unhealthy versus those who are healthy. I am separating that normal weight category into two groups: people who have stable, normal weight throughout adulthood—they have extremely low mortality rates—and people who used to be overweight or obese. And they have quadruple the mortality rate. These are people who are losing weight on their pathway to death due to cardiovascular disease, due to cancer. The fact that their mortality rate is so high indicates that this is not a healthy weight loss.
Flegal’s and almost every other study don’t separate out those different types of normal-weight people. They just lump all those people together and consider them normal weight, such that it seems being overweight and obesity aren’t that bad for you. But that’s just because the normal weight category they are looking at is contaminated with diseased normal-weight subjects.
The next step is to replicate these findings using longitudinal data. In the data I’ve used, the weight histories are based on recall, what the patient said. That is going to be a source of error. My guess is that people generally underestimated what they weighed at their heaviest.
What are the implications of your study?
The bias that my study has uncovered is widely seen in the literature. Katherine Flegal is just summarizing the results from 97 individual studies, which suggests that we really don’t yet appreciate the mortality rate of being overweight and of obesity. We really consistently underestimate it. People shouldn’t be changing their New Year’s resolution in light of Katherine Flegal and her colleagues.
I think that labeling it a disease brings much needed attention to this issue for clinicians. Obesity is an issue that needs to be addressed urgently. The other thing that calling obesity a disease can do is remove some blame from individuals, as a problem that has more complicated roots than individual irresponsibility, individual lack of discipline, laziness.
The data show that not enough doctors are discussing lifestyle modifications with their patients. And calling obesity a disease will position obesity more front and center in the patient-doctor interaction. It is a complicated issue, but I am for it.







































Related Stories
Focusing on Weight May Be Hazardous to Your Health
SPH Bicknell lecturer: what’s wrong with approach to obesity epidemic
Is Obesity a Disease?
American doctors vote yes, BU profs weigh in on debate
Blood Test May Predict Who Lives or Dies with Ebola
Aggressive immune response signals poor outcome
Post Your Comment