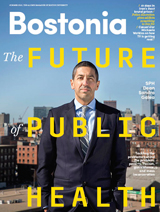
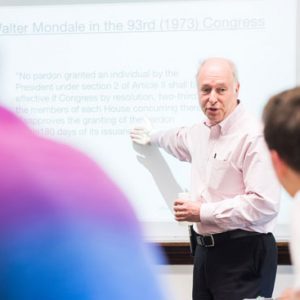
Julie Gerberding inhabits a world of long-winded conference calls and consensus-building meetings.
“Ladies and gentlemen,” the former head of the US Centers for Disease Control and Prevention (CDC) has been known to interject, “people are dying. Let’s step up. Let’s get the decision made. Let’s move on.”
But in offering advice to School of Public Health graduates on May 18, Gerberding, currently president of the vaccine division of pharmaceutical giant Merck, urged the 250 members of the Class of 2013 to temper their passion for change with patience. “Without patience, passion can be reckless, even dangerous,” she said. “It is important to balance the accelerator pedal with the brake of patience, because that is what ultimately helps us be effective.”
The first woman to head the CDC, Gerberding was responsible for coordinating emergency responses to bioterrorism, SARS, West Nile virus, and other health threats during her tenure, from 2002 to 2009. She told the graduates to become “dauntless doers”—undeterred by the magnitude of the public health problems confronting them, but also accepting of the reality that there are no shortcuts or quick fixes.
In her address, she laid out a series of domestic and global health challenges, ranging from malaria to a lack of clean water to the spiraling costs of health care.
“My generation has left you with a gaping hole: we have an enormous global health deficit,” Gerberding said. “We’re not going to solve these global health deficits by health care reform. We’re not going to solve them by more taxes. We’re not going to solve them by new medicine. We’re not going to solve them by…foreign aid or philanthropy.
“These global health deficits have to be solved in new ways—and you have to be the dauntless doers to step up to the plate and figure this out.”
The next generation of public health workers, she said, will have to tackle noncommunicable diseases, such as cancer and obesity, while continuing to battle AIDS, tuberculosis, and malaria. In developing countries, noncommunicable diseases are “rapidly taking over the agenda of health systems in these new democracies and other environments,” Gerberding noted. “They’re sucking the most productive people out of society so that the countries themselves cannot gain an economic foothold and thrive.”
She told the graduates that the key to making an impact in public health was to “translate a dream into doing.” She had set her sights on becoming a physician at an early age, she said, then charted a course that was defined by three principles, grounded in the concept of social justice.
“First of all, I believe that each life is equally valuable. I believe that each learner is equally valiant. And I believe that each leader is equally vital,” she said. “Each of us has to go deep and really define within ourselves our values and principles that make us operate in a way that we feel proud of.”
Before joining the CDC, Gerberding was at the center of the AIDS outbreak in San Francisco in the 1980s, treating patients at San Francisco General Hospital and Trauma Center, and later becoming the hospital’s director of epidemiology. She was director of the National Center for Infectious Diseases before taking over at the CDC, where she was praised for balancing the increased vigilance on bioterrorism with long-standing commitments to AIDS, smoking cessation, and other public health causes. She led the CDC’s response to the anthrax scare of 2001.
An infectious disease specialist, Gerberding called the pursuit of public health an “invisible profession,” saying the public generally does not understand or recognize the behind-the-scenes work that epidemiologists and biostatisticians do—until there is a public health emergency or crisis, such as the April 15 Boston Marathon bombings that claimed 3 lives and injured nearly 300.
“You’re being commenced into the invisible profession—one that is absolutely vital to the health and well-being of people around the world, but one that is usually unnoticed unless there’s a catastrophic outbreak or some other public health emergency and something goes awry,” Gerberding told the graduates.
She encouraged them to take pride in being “stewards of health and well-being and champions of improvement in health disparities. We are the front line of health protection, and we stand strong in the face of public health emergencies like you just experienced here in Boston.”
In welcoming the graduates, SPH Dean Robert Meenan also referred to the Marathon tragedy. The past month had been “a unique and challenging time” for faculty, staff, and students, he said. The aftermath of the Marathon attack presented several “positive take-home messages” for public health, including the importance of focusing on preparedness efforts, the critical role that government plays in responding to emergencies, and the importance of a strong sense of community.
“We saw the importance of community at BUSPH,” Meenan (MED’72, GSM’89) said. “Students turned to one another and to faculty for support. They organized efforts to cope and recover, and to recognize and thank first responders. It was a remarkable, up-close-and-personal object lesson of how a strong, connected community can rise to a challenge.”
Gerberding said daring to dream big was a key quality in public health leadership, citing Jonas Salk’s work on the polio vaccine, former US Surgeon General Luther Terry’s work on tobacco control, and the Accordia Global Health Foundation and Alex Coutinho’s work on HIV/AIDS treatment. But she also pointed to smaller efforts—individual “daring dreamers” like the woman she met on a trip to South Africa who had managed to extricate herself from the sex trade by procuring an old oven and learning to bake bread for sale.
“This is about translating dreams into doing,” she said. “Sadly in the world today, we have many dreamers—but we have precious few doers.”
Despite the myriad challenges in public health, Gerberding said, she remains optimistic that the new generation will make inroads. “We have knowledge, we have tools—and actually, we have a lot of money,” she said.
She called for a new way of thinking about health—not as a “state or condition,” but instead as a “precious natural resource…something that we can quantify.”
“It’s as valuable as oil or clean water or clean air,” she told the Class of 2013.





































Related Stories
State Health and Human Services Secretary SPH Convocation Speaker
Alum Marylou Sudders urges graduates to “search for the positive”
SPH Student Speaker Calls for “Radical Compassion”
Faiz Kidwai urges fellow graduates to be aware of their own privilege
Former Boston TV Anchor Highlights SPH Convocation
Pastor Liz Walker tells students “There is only us”
Post Your Comment