The problem first came to Brian Jack’s attention 10 years ago. The School of Medicine professor and chair of family medicine noticed that patients at Boston Medical Center (BMC), like patients at most hospitals, were leaving without a good understanding of how to care for themselves in the short term. Jack started to track the amount of time that nurses and doctors spent with patients before sending them home. The average was five minutes.
“Patients in the hospital are not at the top of their cognitive game,” says Jack, explaining that sick, feverish, or sleep-deprived people are unlikely to comprehend first-time instructions about prescriptions or at-home care procedures.
Jack and his team found that nearly a third of patients experienced a medical setback after going home, and that one in five returned to the hospital within 30 days. That’s when the team started brainstorming solutions and identified 11 areas that must be covered during each discharge—steps like making appointments for follow-up care, identifying and creating a plan for prescriptions, and educating patients about their diagnoses. That list formed the foundation of Project RED (Reengineered Discharge), a practice that has been shown to lower the rate of returns to the hospital in the month after discharge by 30 percent.
It also led, this fall, to Jack earning the Peter F. Drucker Award for Nonprofit Innovation, a respected prize that has been given annually since 1991 to recognize existing programs that meet famous business guru Drucker’s definition of innovation—“change that creates a new dimension of performance.”
This year, 864 nonprofits applied for the award. Boston Medical Center officials nominated Jack’s Project RED, and it won the top prize of $100,000, which he will accept on behalf of BMC at in a November ceremony in Vienna, Austria.
“Project RED is an example of the innovative work we do here to provide safe, effective care to the whole patient,” says Kate Walsh, BMC president and CEO. “I am extremely proud of Dr. Jack, and the Project RED team, and pleased to see them honored with the Drucker Award for this creative approach to decreasing hospital readmissions.”
These days, before leaving BMC, patients are given a personalized package of information, with details about prescriptions and follow-up appointments, exams, or stress tests color-coded on a calendar. The plan, Jack says, reads like a comic book, with big font sizes, multiple colors, and plenty of icons.

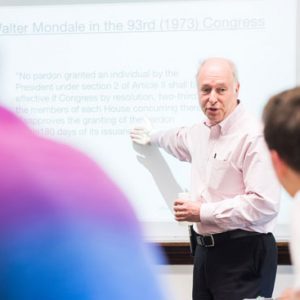
A BMC patient works with Project RED virtual patient advocate Louise to understand her hospital discharge plan. Photo courtesy of Brian Jack
Initially, nurses were responsible for going over each part of the plan with patients, but after they found it was too time-consuming, Jack and Timothy Bickmore, a Northeastern University associate professor of computer and information science, designed a computer program with a virtual patient advocate named Louise, who methodically explains the plan to patients at the end of their hospital stay.
Critics might scoff at Louise’s unpolished animation, but, Jack says, the point isn’t to entertain. “Every time she talks to a patient, it’s about their unique tailored information,” he says. “Louise is still four to five years ahead of her time. That really is the future of health care.”
And that future may have lower system-wide costs. A randomized trial performed in 2009 with 749 patients found a 30 percent lower rate of hospital use in the Project RED intervention group compared to those receiving the usual care one month after a patient’s discharge. One readmission or ER visit was prevented for every seven RED participants. According to Jack’s estimates, if readmission rates can be lowered from the current 20 percent to 15 percent over five years, that would save Medicare $17 billion and the private sector another $17 billion.
Project RED developed “at the right place, at the right time” in terms of federal public policy, Jack says. President Barack Obama’s Affordable Care Act, signed into law in 2010, emphasizes efficiency, reducing hospital readmission rates, and increasing the quality of care and patient safety. Federal agencies are now pushing Project RED as an example among the top 10 best practices for reducing cost while maintaining quality, and Jack estimates that at least 500 hospitals have adopted his team’s new discharge procedure so far.
“Many health care institutions are now studying and implementing Dr. Jack’s Project RED strategies,” says Karen Antman, MED dean and Medical Campus provost. “Clearly, reengineering discharge planning to keep patients safe is key to their recovery and to prevent unneeded readmissions.”
While Jack relishes the national attention and awards Project RED has received, he has other things on his mind—like learning how to waltz and finding something to wear to a formal ball in Vienna.







































Related Stories
MED Physicians among Boston’s Top Docs
Boston magazine’s annual list includes 68 faculty
MED’s Joel Alpert Dies at 83
Pediatrician remembered as strong advocate of primary care
MED Prof Wins Gates Foundation Condom Challenge
$100,000 grant for radiologist’s next-generation design
Post Your Comment